GMJ Medicine
eISSN : 2626-3041
Volume 2, Issue 2 (2023)
GMJM 2023, 2(2): 39-42 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/11/5 | Accepted: 2023/05/26 | Published: 2023/06/29
Received: 2022/11/5 | Accepted: 2023/05/26 | Published: 2023/06/29
How to cite this article
Noei Alamdary S, Ghasembaglou S. Uncommon Pharyngeal Tumors; an Epidemiological Study from 2017 to 2019. GMJM 2023; 2 (2) :39-42
URL: http://gmedicine.de/article-2-186-en.html
URL: http://gmedicine.de/article-2-186-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
Sh. Noei Alamdary1, Sh. Ghasembaglou *1
1- Department of Otorhinolaryngology, School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Keywords:
| Abstract (HTML) (1392 Views)
Full-Text: (345 Views)
Introduction
Head and neck tumors are divided into four general categories: oral, pharyngeal, laryngeal, and salivary glands, which have different prevalence depending on the location of the lesion, so that tumors of the pharyngeal region are rare cases of head and neck tumors [1]. Concerning the clinical importance of examining pharyngeal tumors, it is enough that malignant pharyngeal tumors are always challenging points both in terms of diagnosis and treatment [2].
In 2000, head and neck cancers were the eighth most common cause of cancer death worldwide, with 48,100 new cases and 320,000 deaths this year epidemiologically in pharyngeal tumors, urofacial tumors, and Epidemiological criterion of the hypopharynx. They are uniform, but in the case of nasopharyngeal tumors, its prevalence is higher in Asia, the main reason being the association with the Epstein-Barr virus [3, 4].
Nasopharyngeal tumors are one of the relatively important causes of death in Indonesia because in the initial diagnosis of this disease 80% of patients are in advanced stage of cancer, one of the reasons is the poor knowledge of general practitioners about the early symptoms and viral causes of this carcinoma [5].
Given the above and the increasing prevalence of pharyngeal tumors in recent years and the high mortality of patients with these tumors, the need for epidemiological studies to determine the causes and pathophysiology of these tumors are necessary; Therefore, the present study was performed to investigate the epidemiology of uncommon pharyngeal tumors.
Instrument and Methods
This study is a retrospective cohort that was conducted during the years 2017 to 2019 by reviewing the clinical records of patients referred to the hospitals of Tabriz University of Medical Sciences. Patients were admitted to the study by available sampling method using inclusion/ exclusion criteria. Due to the fact that the sampling method in this study was census, all patients (60 patients) were included in this study. Our criterion for reviewing files was based on the pathological diagnosis of the disease following tumor biopsy, so it is clear that files that did not report pathology were eventually excluded.
Based on the codes defined in the International Statistical Classification of Diseasesand Related health Problems 10th revision, codes related to each of the rare throat diseases are extracted; These codes were as follows: 1. C13.9 hypopharynx (unspecified) includinghypopharyngeal wall NOS 2. C14.0 pharynx (unspecified) 3. D37.0 lip, oral cavity and pharynx 4. D10.6 pharyngeal tonsil involving posteriormargin of septum and choanae A checklist was designed for each disease; The checklist included questions such as gender, age, body mass index, smoking, diabetes mellitus, hypertension and a history of cancer. These questions were asked for each group of codes mentioned above and their epidemiology was examined.
The obtained data were entered into SPSS 21 software. Mean and standard deviation-percentage and frequency were used to display the data. T-test and Chi-square test were used to examine the relationships between the obtained data. The P value in all cases was considered significant for values less than 0.05.
The information extracted from the files was extracted with the utmost honesty; Patients' personal information was not included in the study and incomplete files were not included in the study.
Findings
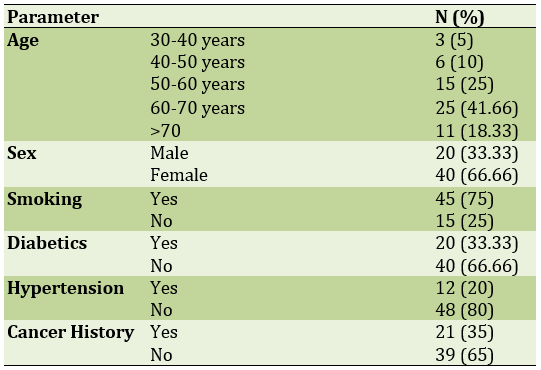
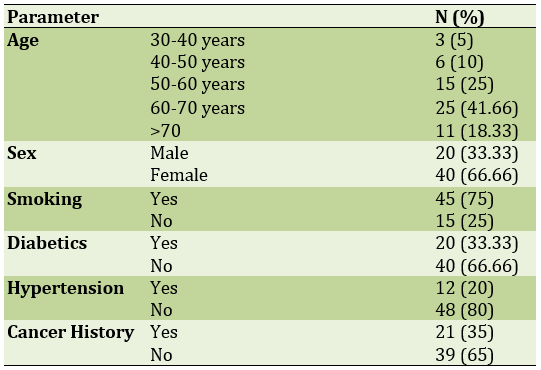
This study was performed on 60 patients. The mean age of participants was 61.42±3.69 years and the majority of them (41 cases) were male. The mean body mass index was 27.14±1.91. There was a history of cancer in 21 patients (Table 1).
Table 1) Examination of demographic information of study participants
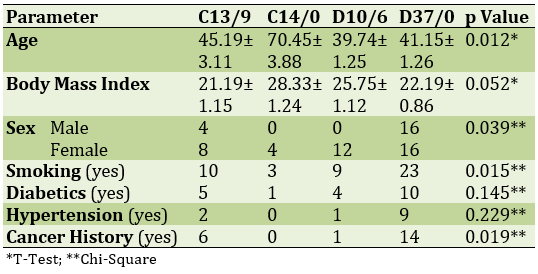
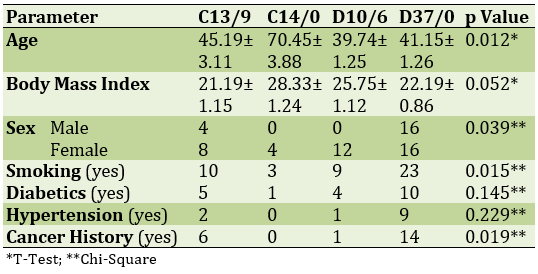
The lowest type of cancer in the studied cases was C14/0 and the highest type of cancer was D37/0 The mean age in group C14/0 was significantly higher than other groups and in group D37/0. male gender had the most conflict. In all cancers, female gender was the most common; The highest smoking rate was in the D37/0 group (Table 2).
Table 2) Clinical epidemiology of uncommon pharyngeal cancers
Discussion
Having throat cancer in people can have different signs and symptoms. The patient may suspect a lump in his or her neck, or his or her hearing may be impaired, which usually occurs in only one ear. Tinnitus is another possible symptom of nasopharyngeal cancer, in which a bell-like sound is produced from inside the body. They may also have nosebleeds or nasal congestion. Localized pain is not common in this type of cancer, but the presence of an Eustachian tube hole in the nasopharynx plays a major role in the development of symptoms of nasopharyngeal cancer in the nasal cavity. The pressure in the nasopharynx on the opening of the Eustachian tube does not allow it to open, as a result of which fluid collects in the middle ear and the patient will develop otitis media with fluid leakage. In this case, the patient will feel a fullness of the ear and a slight to moderate hearing loss, in which case there is mostly no pain, unless the ear fluid becomes secondarily infected [5-8].
The importance of examining neoplasms of the pharyngeal region is because there are no serious and obvious symptoms of these tumors except in the late and advanced stages [9]. A tumor that has grown in the throat may interfere with hearing, smell, taste, speech and swallowing. In these cases, the person may have difficulty swallowing with pain, coughing up blood, blood in the saliva, white patches in the mouth, earache, or a feeling of tightness and closure of the ear, a hard lump in the throat or lymph nodes in the neck. Swelling of the lymph nodes in the neck. A tumor that is localized in the back of the nose causes nosebleeds, tinnitus, pain, or a feeling of pressure in the middle ear [3, 10].
The symptoms of laryngeal cancer mainly depend on the size and location of the tumor. Most laryngeal cancers start in the vocal cords. These tumors are rarely painful, but will almost always cause hoarseness (violence) or other changes in sound. Tumors in the area above the vocal cords may cause a bulge in the neck, sore throat, or earache [8]. Tumors that start in the lower part of the vocal cords are very rare. Such tumors will make it difficult to breathe and cause chest tightness or shortness of breath. Chronic coughs or a feeling of bloating and sore throat can also be signs of laryngeal cancer, and as the tumor grows, they may cause pain, weight loss, bad breath, and recurrent suffocation when eating. In some cases, a tumor that grows in the larynx can make swallowing difficult. All of these symptoms may be caused by cancer or other less serious problems. People who experience such symptoms usually see an ear, nose and throat specialist [11-13].
Risk factors for nasopharyngeal cancer, including smoking - Eating certain foods increases the risk of nasopharyngeal cancer. This cancer is more prevalent in Asia and South Africa [14]. People in these areas have a salty diet rich in nitrates and nitrites, which in response to protein form a substance called nitrosamines, which can cause cellular DNA damage. People with a family history of nasopharyngeal cancer The incidence of this cancer is higher. People who come in contact with wood particles at work are more likely to develop nasopharyngeal cancer. It can also be caused by inhaling wood particles. People with ENT conditions can be at risk for nasopharyngeal cancer. Which can be accompanied by symptoms such as runny nose, middle ear infection or polyps [15-17].
The limitations of this study were the small sample size and the lack of evaluation of all patients suspected of cancer, as well as the lack of intervention and the history of chemotherapy and radiotherapy. For future studies, it is suggested that the limitations of this study be removed. Also, to determine the comprehensive pattern of pharyngeal tumors in Iran, it is recommended to conduct a study in other provinces of Iran.
Conclusion
Pharyngeal tumors are as rare in northwestern Iran as in other parts of the world. However, this study found that these tumors appear with different clinical and pathological symptoms. Smoking, old age, previous history of cancer are the risk factors for this disease.
Acknowledgements: None declared by the authors.
Ethical Permission: This study has been approved by the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1397.294).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
Head and neck tumors are divided into four general categories: oral, pharyngeal, laryngeal, and salivary glands, which have different prevalence depending on the location of the lesion, so that tumors of the pharyngeal region are rare cases of head and neck tumors [1]. Concerning the clinical importance of examining pharyngeal tumors, it is enough that malignant pharyngeal tumors are always challenging points both in terms of diagnosis and treatment [2].
In 2000, head and neck cancers were the eighth most common cause of cancer death worldwide, with 48,100 new cases and 320,000 deaths this year epidemiologically in pharyngeal tumors, urofacial tumors, and Epidemiological criterion of the hypopharynx. They are uniform, but in the case of nasopharyngeal tumors, its prevalence is higher in Asia, the main reason being the association with the Epstein-Barr virus [3, 4].
Nasopharyngeal tumors are one of the relatively important causes of death in Indonesia because in the initial diagnosis of this disease 80% of patients are in advanced stage of cancer, one of the reasons is the poor knowledge of general practitioners about the early symptoms and viral causes of this carcinoma [5].
Given the above and the increasing prevalence of pharyngeal tumors in recent years and the high mortality of patients with these tumors, the need for epidemiological studies to determine the causes and pathophysiology of these tumors are necessary; Therefore, the present study was performed to investigate the epidemiology of uncommon pharyngeal tumors.
Instrument and Methods
This study is a retrospective cohort that was conducted during the years 2017 to 2019 by reviewing the clinical records of patients referred to the hospitals of Tabriz University of Medical Sciences. Patients were admitted to the study by available sampling method using inclusion/ exclusion criteria. Due to the fact that the sampling method in this study was census, all patients (60 patients) were included in this study. Our criterion for reviewing files was based on the pathological diagnosis of the disease following tumor biopsy, so it is clear that files that did not report pathology were eventually excluded.
Based on the codes defined in the International Statistical Classification of Diseasesand Related health Problems 10th revision, codes related to each of the rare throat diseases are extracted; These codes were as follows: 1. C13.9 hypopharynx (unspecified) includinghypopharyngeal wall NOS 2. C14.0 pharynx (unspecified) 3. D37.0 lip, oral cavity and pharynx 4. D10.6 pharyngeal tonsil involving posteriormargin of septum and choanae A checklist was designed for each disease; The checklist included questions such as gender, age, body mass index, smoking, diabetes mellitus, hypertension and a history of cancer. These questions were asked for each group of codes mentioned above and their epidemiology was examined.
The obtained data were entered into SPSS 21 software. Mean and standard deviation-percentage and frequency were used to display the data. T-test and Chi-square test were used to examine the relationships between the obtained data. The P value in all cases was considered significant for values less than 0.05.
The information extracted from the files was extracted with the utmost honesty; Patients' personal information was not included in the study and incomplete files were not included in the study.
Findings
This study was performed on 60 patients. The mean age of participants was 61.42±3.69 years and the majority of them (41 cases) were male. The mean body mass index was 27.14±1.91. There was a history of cancer in 21 patients (Table 1).
Table 1) Examination of demographic information of study participants
The lowest type of cancer in the studied cases was C14/0 and the highest type of cancer was D37/0 The mean age in group C14/0 was significantly higher than other groups and in group D37/0. male gender had the most conflict. In all cancers, female gender was the most common; The highest smoking rate was in the D37/0 group (Table 2).
Table 2) Clinical epidemiology of uncommon pharyngeal cancers
Discussion
Having throat cancer in people can have different signs and symptoms. The patient may suspect a lump in his or her neck, or his or her hearing may be impaired, which usually occurs in only one ear. Tinnitus is another possible symptom of nasopharyngeal cancer, in which a bell-like sound is produced from inside the body. They may also have nosebleeds or nasal congestion. Localized pain is not common in this type of cancer, but the presence of an Eustachian tube hole in the nasopharynx plays a major role in the development of symptoms of nasopharyngeal cancer in the nasal cavity. The pressure in the nasopharynx on the opening of the Eustachian tube does not allow it to open, as a result of which fluid collects in the middle ear and the patient will develop otitis media with fluid leakage. In this case, the patient will feel a fullness of the ear and a slight to moderate hearing loss, in which case there is mostly no pain, unless the ear fluid becomes secondarily infected [5-8].
The importance of examining neoplasms of the pharyngeal region is because there are no serious and obvious symptoms of these tumors except in the late and advanced stages [9]. A tumor that has grown in the throat may interfere with hearing, smell, taste, speech and swallowing. In these cases, the person may have difficulty swallowing with pain, coughing up blood, blood in the saliva, white patches in the mouth, earache, or a feeling of tightness and closure of the ear, a hard lump in the throat or lymph nodes in the neck. Swelling of the lymph nodes in the neck. A tumor that is localized in the back of the nose causes nosebleeds, tinnitus, pain, or a feeling of pressure in the middle ear [3, 10].
The symptoms of laryngeal cancer mainly depend on the size and location of the tumor. Most laryngeal cancers start in the vocal cords. These tumors are rarely painful, but will almost always cause hoarseness (violence) or other changes in sound. Tumors in the area above the vocal cords may cause a bulge in the neck, sore throat, or earache [8]. Tumors that start in the lower part of the vocal cords are very rare. Such tumors will make it difficult to breathe and cause chest tightness or shortness of breath. Chronic coughs or a feeling of bloating and sore throat can also be signs of laryngeal cancer, and as the tumor grows, they may cause pain, weight loss, bad breath, and recurrent suffocation when eating. In some cases, a tumor that grows in the larynx can make swallowing difficult. All of these symptoms may be caused by cancer or other less serious problems. People who experience such symptoms usually see an ear, nose and throat specialist [11-13].
Risk factors for nasopharyngeal cancer, including smoking - Eating certain foods increases the risk of nasopharyngeal cancer. This cancer is more prevalent in Asia and South Africa [14]. People in these areas have a salty diet rich in nitrates and nitrites, which in response to protein form a substance called nitrosamines, which can cause cellular DNA damage. People with a family history of nasopharyngeal cancer The incidence of this cancer is higher. People who come in contact with wood particles at work are more likely to develop nasopharyngeal cancer. It can also be caused by inhaling wood particles. People with ENT conditions can be at risk for nasopharyngeal cancer. Which can be accompanied by symptoms such as runny nose, middle ear infection or polyps [15-17].
The limitations of this study were the small sample size and the lack of evaluation of all patients suspected of cancer, as well as the lack of intervention and the history of chemotherapy and radiotherapy. For future studies, it is suggested that the limitations of this study be removed. Also, to determine the comprehensive pattern of pharyngeal tumors in Iran, it is recommended to conduct a study in other provinces of Iran.
Conclusion
Pharyngeal tumors are as rare in northwestern Iran as in other parts of the world. However, this study found that these tumors appear with different clinical and pathological symptoms. Smoking, old age, previous history of cancer are the risk factors for this disease.
Acknowledgements: None declared by the authors.
Ethical Permission: This study has been approved by the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1397.294).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
References
1. Wu L, Li C, Pan L. Nasopharyngeal carcinoma: A review of current updates. Exp Ther Med. 2018;15(4):3687-92. [Link] [DOI:10.3892/etm.2018.5878]
2. Nour AS, Weldehawariat TD, Woldemariam AA, Layo DG. nasopharyngeal carcinoma: a retrospective study on imaging patterns at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. Ethiop J Health Sci. 2020;30(2):215-22. [Link] [DOI:10.4314/ejhs.v30i2.9]
3. Wahyuningsih L, Dwianingsih EK, Risanti ED, Tirtoprodjo P, Rinonce HT, Hakim FA, et al. Asian Pac J Cancer Prev. 2019;20(7):2125-30. [Link] [DOI:10.31557/APJCP.2019.20.7.2125]
4. Ogun GO, Olusanya AA, Akinmoladun VI, Adeyemo AA, Ogunkeyede SA, Daniel A, et al. Nasopharyngeal carcinoma in Ibadan, Nigeria: a clinicopathologic study. Pan Afr Med J . 2020;36:82. [Link] [DOI:10.11604/pamj.2020.36.82.19657]
5. Abraham Z, Ntunaguzi D, Kahinga AA, Massawe ER. Clinico-pathological profile of nasopharyngeal carcinoma at Muhimbili national hospital, Dares Salaam, Tanzania. nt J Otorhinolaryngol Head Neck Surg.2019;5(4):922-5. [Link] [DOI:10.18203/issn.2454-5929.ijohns20192705]
6. Chen YP, Chan AT, Le QT, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet. 2019;394(10192):64-80. [Link] [DOI:10.1016/S0140-6736(19)30956-0]
7. Memirie ST. Estimates of Cancer Incidence in Ethiopia in 2015 using population-based registry data. J Glob Oncol.2018;4(4):1-11. [Link] [DOI:10.1200/JGO.17.00175]
8. Chua ML, Wee JT, Hui EP, Chan AT. Nasopharyngeal carcinoma. Lancet. 2016 ;387(10022):1012-24. [Link] [DOI:10.1016/S0140-6736(15)00055-0]
9. Acuña G, Gomà M, Temprana-Salvador J, Garcia-Bragado F, Alós L, Ordi J, et al. Human papillomavirus in laryngeal and hypopharyngeal lymphoepithelial carcinoma. Mod Pathol. 2019;32(5):621-6. [Link] [DOI:10.1038/s41379-018-0188-2]
10. Virgilio AD, Costantino A, Mercante G, Maio PD, Iocca O, Spriano G. Trans-oral robotic surgery in the management of parapharyngeal space tumors: A systematic review. Oral Oncol. 2020;103:104581. [Link] [DOI:10.1016/j.oraloncology.2020.104581]
11. Torabi SJ, Cheraghlou S, Kasle D, Savoca EL, Judson BL. Nonsquamous cell laryngeal cancers: Incidence, demographics, care patterns, and effect of surgery. Laryngoscope. 2019;129(11):2496-505. [Link] [DOI:10.1002/lary.27785]
12. El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ. WHO Classification of Head and Neck Tumours. 4th ed. WHO: Geneva;2017. [Link]
13. Wong MYW, Wang B, Yang A, Khor A, Xuan W, Rajendra S. Human papillomavirus exposure and sexual behavior are significant risk factors for Barrett's dysplasia/esophageal adenocarcinoma. Dis Esophagus. 2018;31(12):1-8. [Link] [DOI:10.1093/dote/doy051]
14. Tsikouras P, Zervoudis S, Manav B, Tomara E, Iatrakis G, Romanidis C, et al. Cervical cancer: Screening, diagnosis and staging. J BUON. 2016;21(2):320-5. [Link]
15. Yamashina T, Shimatani M, Takeo M, Sasaki K, Orino M, Saito N, et al. Viral infection in esophageal, gastric, and colorectal cancer. Healthcare (Basel). 2022;10(9):1626. [Link] [DOI:10.3390/healthcare10091626]
16. El-Zimaity H, Pilato VD, Ringressi MN, Brcic I, Rajendra S, Langer R, et al. Ann N Y Acad Sci. 2018;1434(1):319-32. [Link] [DOI:10.1111/nyas.13858]
17. Sellami K, Mseddi M, Snoussi M, Gharbi H, Frikha F, Salah RB, Jallouli M, et al. Malignancy in a retrospective cohort of 17 patients with Dermatomyositis or Polymyositis in southern Tunisia. Rom J Intern Med. 2018;56(4):243-9. [Link] [DOI:10.2478/rjim-2018-0015]