GMJ Medicine
eISSN : 2626-3041
Volume 2, Issue 2 (2023)
GMJM 2023, 2(2): 57-61 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/09/12 | Accepted: 2023/03/1 | Published: 2023/04/23
Received: 2022/09/12 | Accepted: 2023/03/1 | Published: 2023/04/23
How to cite this article
Maroufi P, Nazari B. Radiography Need in Patients with Shoulder Dislocations; Case Study of Shohada Hospital, Iran. GMJM 2023; 2 (2) :57-61
URL: http://gmedicine.de/article-2-190-en.html
URL: http://gmedicine.de/article-2-190-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
P. Maroufi1, B. Nazari *2
1- Department of Orthopedics, School of Medicine, Shohada Medical Research & Training Hospital, Tabriz University of Medical Sciences, Tabriz, Iran
2- Department of Orthopedics, School of Medicine, Rahat Breath and Sleep Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2- Department of Orthopedics, School of Medicine, Rahat Breath and Sleep Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Keywords:
| Abstract (HTML) (1358 Views)
Full-Text: (390 Views)
Introduction
Anterior shoulder dislocation is the most common joint dislocation in humans. Its prevalence in the community is 17 per 100,000. Manifestations include severe pain and the patient's inability to perform certain shoulder movements [1]. The affected hand is on one side away from the body and the forearm is turned outwards [2]. Sometimes the head of the humerus is touched anteriorly. In some cases, this dislocation is accompanied by fractures such as anterior glenoid fractures and large tuberosity of the humerus. Diagnosis of this type of dislocation can be easily done by taking a history and a thorough physical examination [3].
Closed reduction of this dislocation is usually successful. Studies have shown that the probability of reduction failure is between 0 and 30% [4]. There are several methods to reduce this dislocation such as Hippocratic method, Milch method, Stimson method and Scapular manipulation [5]. Reduction of this dislocation in hospitals is done by orthopedic or emergency specialists. In most cases, both of these doctors request a radiograph of the shoulder before and after the reduction procedure [6]. Reasons for requesting these radiographs include confirmation of dislocation, complete reduction, and ensuring that no new fractures occur during shoulder reduction [7].
Studies have shown very few cases of fractures following reduction of shoulder dislocations. In fact, in many studies, the possibility of fractures following reduction has been reported to be very rare [8-10]; Especially when the reduction is done with more modern methods and with less chance of damage. Recent studies have questioned pre- and post-reduction radiography in all cases of anterior shoulder dislocation. Numerous studies have been conducted in this field. In these studies, some of which were retrospective and some of which were prospective, the researchers concluded that because the physician's diagnostic accuracy in determining the presence of dislocation and reduction is very high, pre- and post-reduction radiography is not necessary for all cases of shoulder dislocation. Cases where the doctor is sure there is a complete dislocation or reduction can be ignored [11-14]. However, in cases where the doctor is not sure of complete reduction, radiography is recommended for control. Also, in these studies following reduction, even in cases with fractures, no significant new fractures were seen in control radiography [15].
Due to the fact that radiography before and after reduction requires significant waste of time, the patient is exposed to harmful radiation and imposes a significant material burden on patients, the present study was conducted based on these objectives to see if the physician's clinical judgment in determining the presence of anterior shoulder dislocation is so accurate that preoperative radiography can be ruled out in these patients. Positive results, improvements in the process of diagnosis and treatment of these patients.
Instrument and Methods
Study design
This cross-sectional descriptive study was conducted during 2019 in Shohada Hospital (Tabriz University of Medical Sciences) with the participation of patients referred to the hospital emergency department. Using the results of a similar study, the sample size was considered equal to 0.05, β equal to 2, the strength of the study equal to 80%, and the sample loss of about ten percent was considered equal to 116 patients. Patients were admitted to the study by observing the inclusion and exclusion criteria as well as by available and purposeful sampling methods.
Inclusion/Exclusion Criteria
Inclusion criteria included individuals who had pain following a shoulder injury or spontaneous pain and limited movement of the shoulder joint by abduction and external rotation of the joint with a possible diagnosis of anterior dislocation of the shoulder joint were included in the study. Exclusion criteria included: age over 65 and under 15 years and the presence of bone, nerve or vascular damage in the affected limb.
Procedure
Patients were examined before radiography by specialists or senior residents of emergency medicine. Demographic information, cause of dislocation (traumatic or non-traumatic), degree of dislocation (first or repeated) and physician diagnosis (definitive or suspected dislocation) were recorded. Radiography was performed and sent to an orthopedist. If the dislocation is confirmed by an orthopedist, the reduction was performed as desired by the emergency physician. Examination of the shoulder joint, hearing the clicking of the bone as it moved, and the patient feeling pain were used to confirm the reduction. The overall evaluation result was written as complete, suspicious or unsuccessful reduction. The control radiograph was then taken and sent back to the orthopedist for consultation. If the orthopedist is confirmed, the shoulder is closed and the patient is discharged with the recommendation to visit an orthopedic clinic. In cases of incomplete reduction, the patient was sent to the operating room. Finally, the emergency physician's diagnosis was compared with the orthopedist's view of dislocation, reduction, and fracture.
Data analysis
The obtained data were entered into SPSS 21 software, descriptive statistical methods were used to display the data and t-test was used to compare the results.
Ethical considerations
Written consent was obtained from all patients. The objectives of the study were explained to the patients in simple and understandable language so that they could enter the study if they were satisfied.
Findings
84 of the subjects (72%) were male and 32 (28%) were female. The mean age of study participants was 31.49±5.74 years; 30 patients had recurrent shoulder dislocation with non-traumatic mechanism (group 1) and 86 patients had the first case of shoulder dislocation or dislocation with traumatic mechanism (group 2).
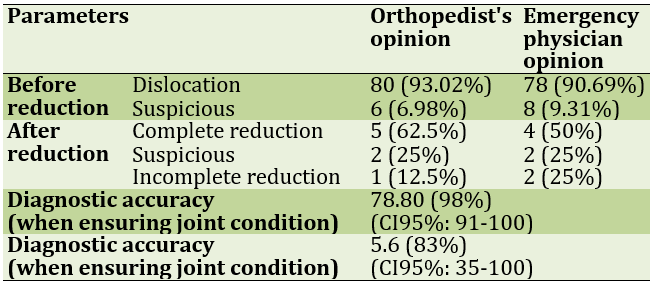
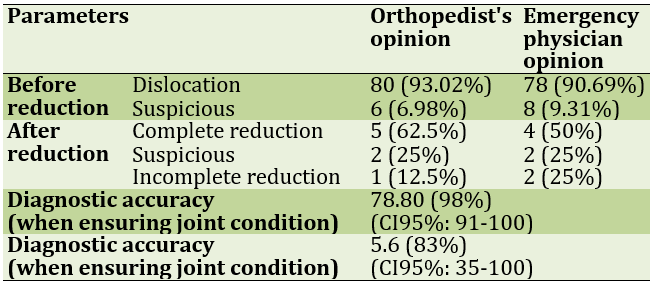
In group 1, there were no fractures before and after reduction of 8 cases. There were fractures in cases with group 2 trauma, but no new fractures were seen in all cases after reduction. In group 1, one case and in group 2, six cases of unsuccessful reduction were sent to the operating room (Tables 1 and 2).
Table 1) Careful examination of the physician in determining the position of the joint in the group with repeated dislocation of the shoulder with a non-traumatic mechanism
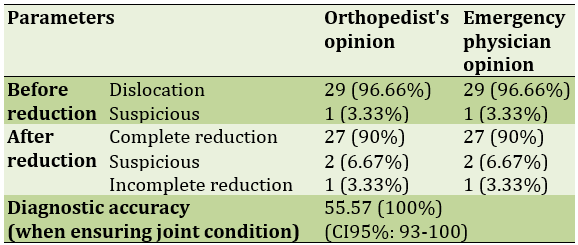
Table 2) Accuracy of physician examination in determining the position of the joint in the group with the first dislocation or with the mechanism of impact
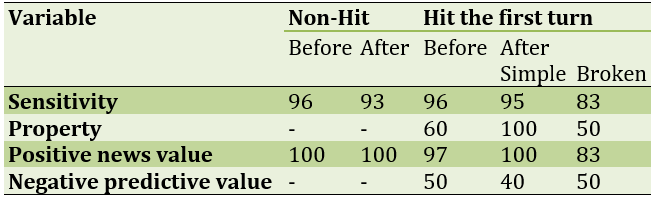
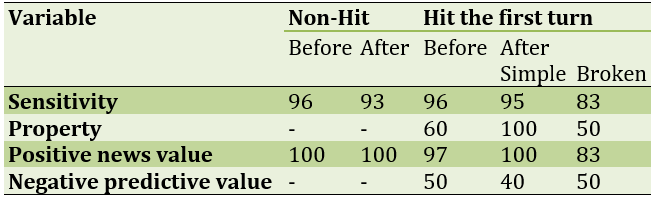
The statistical values of the physician examination are shown in Table 3.
Table 3) Statistical values of emergency physician examination in determining the condition of the shoulder joint
Discussion
The present study showed that in cases of recurrent anterior shoulder dislocations without impact mechanism, physicians were able to accurately diagnose dislocations and correct reduction. In cases where the definitive diagnosis of the emergency physician was complete dislocation or reduction, orthopedic approval was observed in all cases (100% diagnostic accuracy). There was no significant difference between the opinion of the physician and the orthopedist when the emergency physician was sure of the joint condition. Therefore, it can be concluded that in cases of recurrent anterior shoulder dislocation without impact mechanism, radiography before and after reduction can be omitted [16-18].
In the case of first-time dislocation or with the mechanism of impact, unlike the first group, more cases of dislocation of the physician were observed that 50% of the suspected cases were not dislocated according to the orthopedist. However, in this group, when the emergency physician was sure of the joint condition, there was no significant difference between the opinion of the physician and the orthopedist [15-17].
On the other hand, 8 fractures were seen in group 2, which was a significant number of cases with dislocation-fracture in patients with unsuccessful reduction or uncertainty of joint condition after reduction. The physician's diagnostic accuracy was significantly lower than the reduction status in these individuals. There was a significant difference between the opinion of the physician and the orthopedist, so in cases with fractures, radiography should be performed after reduction because in these cases, it is difficult to assess the condition of the joint with examination [19, 20].
In group 2 patients whose radiographs did not have fractures, we again saw very high diagnostic accuracy of physicians at full confidence (100%); There was no significant difference between the opinion of the physician and the orthopedist. Therefore, we conclude that in cases of first shoulder dislocation or by impact mechanism, if no fracture is seen in pre-reduction radiography, post-reduction radiography can be removed if the physician is sure of complete reduction [21-23].
Today, doctors routinely request radiographs of the shoulder before and after reduction of the anterior shoulder dislocation. Performing radiography before and after anterior shoulder reduction is one of the topics discussed by orthopedic and emergency medicine specialists. A group of researchers believe that this dislocation can be easily detected by taking a history and detailed examination. Other studies, on the other hand, have questioned post-reduction radiography. In these studies, reducing pain, hearing reduction clicks, and improving range of motion of the joint instead of radiographs have been recommended [23-26].
The percentage of reduction in shoulder dislocation, regardless of the type of reduction technique, is 70 to 96%. The reduction success rate in this study was 94%. In two studies performed on 69 and 104 patients, 2 and 5 reduction failures occurred, respectively. This was 7 cases in our study, which may be due to age and physical differences of patients or due to greater caution and consideration, in order not to cause secondary damage during reduction in our study. In the two studies, no significant new fractures were seen following reduction, which is consistent with the results of the present study [27-29].
Several researchers have studied the need for radiography before and after shoulder dislocation reduction. These doctors developed an algorithm for the need for radiography. According to this algorithm, the radiograph of the shoulder in the case of the first dislocation, cases with trauma and uncertainty of the doctor of the joint position were taken. With this algorithm, a 46% reduction in radiographs and significant time savings were observed. On the other hand, no case of fracture or missing dislocation was found in cases without shoulder radiography (by telephone follow-up). Finally, the researchers concluded that the physician's opinion in determining the location of the humerus is very accurate, so in case of shoulder dislocation, radiography should be requested selectively and according to the recommended algorithm [29-31].
Another study on postoperative radiographic value was performed on 73 patients with anterior shoulder dislocation. In this study, about 37% of fractures were seen only in post-reduction radiography, however, none of these missed fractures interfered with the treatment of dislocation. The researchers concluded that anterior shoulder dislocations may be associated with fractures that are not seen on primary radiography due to the small size or position of the joint, but these fractures do not change the patient's healing process [31].
This study has some limitations. A number of eligible patients may not be included in the study due to lack of diagnosis by the physician (false negative), physicians' skills in examining the shoulder joint vary, and on the other hand, a number of small fractures may not be seen on radiography.
Conclusion
Physicians are able to accurately diagnose dislocation and reduction in cases of non-fracture shoulder dislocations. Shoulder radiography should be requested at a time when the physician is unsure of the condition of the joint. In the first dislocation or with the mechanism of radiographic shock should be done before reduction. In these patients, postoperative radiography should be limited to cases with fractures or suspected. Therefore, when the physician determines the condition of the shoulder joint through examination and history, shoulder radiography does not add a new point that changes the patient's treatment process.
Acknowledgements: None declared by the authors.
Ethical Permission: This study was performed after approval by the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.1250).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
Anterior shoulder dislocation is the most common joint dislocation in humans. Its prevalence in the community is 17 per 100,000. Manifestations include severe pain and the patient's inability to perform certain shoulder movements [1]. The affected hand is on one side away from the body and the forearm is turned outwards [2]. Sometimes the head of the humerus is touched anteriorly. In some cases, this dislocation is accompanied by fractures such as anterior glenoid fractures and large tuberosity of the humerus. Diagnosis of this type of dislocation can be easily done by taking a history and a thorough physical examination [3].
Closed reduction of this dislocation is usually successful. Studies have shown that the probability of reduction failure is between 0 and 30% [4]. There are several methods to reduce this dislocation such as Hippocratic method, Milch method, Stimson method and Scapular manipulation [5]. Reduction of this dislocation in hospitals is done by orthopedic or emergency specialists. In most cases, both of these doctors request a radiograph of the shoulder before and after the reduction procedure [6]. Reasons for requesting these radiographs include confirmation of dislocation, complete reduction, and ensuring that no new fractures occur during shoulder reduction [7].
Studies have shown very few cases of fractures following reduction of shoulder dislocations. In fact, in many studies, the possibility of fractures following reduction has been reported to be very rare [8-10]; Especially when the reduction is done with more modern methods and with less chance of damage. Recent studies have questioned pre- and post-reduction radiography in all cases of anterior shoulder dislocation. Numerous studies have been conducted in this field. In these studies, some of which were retrospective and some of which were prospective, the researchers concluded that because the physician's diagnostic accuracy in determining the presence of dislocation and reduction is very high, pre- and post-reduction radiography is not necessary for all cases of shoulder dislocation. Cases where the doctor is sure there is a complete dislocation or reduction can be ignored [11-14]. However, in cases where the doctor is not sure of complete reduction, radiography is recommended for control. Also, in these studies following reduction, even in cases with fractures, no significant new fractures were seen in control radiography [15].
Due to the fact that radiography before and after reduction requires significant waste of time, the patient is exposed to harmful radiation and imposes a significant material burden on patients, the present study was conducted based on these objectives to see if the physician's clinical judgment in determining the presence of anterior shoulder dislocation is so accurate that preoperative radiography can be ruled out in these patients. Positive results, improvements in the process of diagnosis and treatment of these patients.
Instrument and Methods
Study design
This cross-sectional descriptive study was conducted during 2019 in Shohada Hospital (Tabriz University of Medical Sciences) with the participation of patients referred to the hospital emergency department. Using the results of a similar study, the sample size was considered equal to 0.05, β equal to 2, the strength of the study equal to 80%, and the sample loss of about ten percent was considered equal to 116 patients. Patients were admitted to the study by observing the inclusion and exclusion criteria as well as by available and purposeful sampling methods.
Inclusion/Exclusion Criteria
Inclusion criteria included individuals who had pain following a shoulder injury or spontaneous pain and limited movement of the shoulder joint by abduction and external rotation of the joint with a possible diagnosis of anterior dislocation of the shoulder joint were included in the study. Exclusion criteria included: age over 65 and under 15 years and the presence of bone, nerve or vascular damage in the affected limb.
Procedure
Patients were examined before radiography by specialists or senior residents of emergency medicine. Demographic information, cause of dislocation (traumatic or non-traumatic), degree of dislocation (first or repeated) and physician diagnosis (definitive or suspected dislocation) were recorded. Radiography was performed and sent to an orthopedist. If the dislocation is confirmed by an orthopedist, the reduction was performed as desired by the emergency physician. Examination of the shoulder joint, hearing the clicking of the bone as it moved, and the patient feeling pain were used to confirm the reduction. The overall evaluation result was written as complete, suspicious or unsuccessful reduction. The control radiograph was then taken and sent back to the orthopedist for consultation. If the orthopedist is confirmed, the shoulder is closed and the patient is discharged with the recommendation to visit an orthopedic clinic. In cases of incomplete reduction, the patient was sent to the operating room. Finally, the emergency physician's diagnosis was compared with the orthopedist's view of dislocation, reduction, and fracture.
Data analysis
The obtained data were entered into SPSS 21 software, descriptive statistical methods were used to display the data and t-test was used to compare the results.
Ethical considerations
Written consent was obtained from all patients. The objectives of the study were explained to the patients in simple and understandable language so that they could enter the study if they were satisfied.
Findings
84 of the subjects (72%) were male and 32 (28%) were female. The mean age of study participants was 31.49±5.74 years; 30 patients had recurrent shoulder dislocation with non-traumatic mechanism (group 1) and 86 patients had the first case of shoulder dislocation or dislocation with traumatic mechanism (group 2).
In group 1, there were no fractures before and after reduction of 8 cases. There were fractures in cases with group 2 trauma, but no new fractures were seen in all cases after reduction. In group 1, one case and in group 2, six cases of unsuccessful reduction were sent to the operating room (Tables 1 and 2).
Table 1) Careful examination of the physician in determining the position of the joint in the group with repeated dislocation of the shoulder with a non-traumatic mechanism
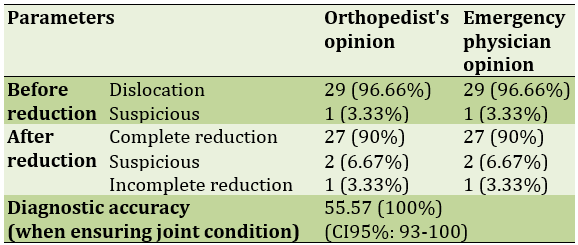
Table 2) Accuracy of physician examination in determining the position of the joint in the group with the first dislocation or with the mechanism of impact
The statistical values of the physician examination are shown in Table 3.
Table 3) Statistical values of emergency physician examination in determining the condition of the shoulder joint
Discussion
The present study showed that in cases of recurrent anterior shoulder dislocations without impact mechanism, physicians were able to accurately diagnose dislocations and correct reduction. In cases where the definitive diagnosis of the emergency physician was complete dislocation or reduction, orthopedic approval was observed in all cases (100% diagnostic accuracy). There was no significant difference between the opinion of the physician and the orthopedist when the emergency physician was sure of the joint condition. Therefore, it can be concluded that in cases of recurrent anterior shoulder dislocation without impact mechanism, radiography before and after reduction can be omitted [16-18].
In the case of first-time dislocation or with the mechanism of impact, unlike the first group, more cases of dislocation of the physician were observed that 50% of the suspected cases were not dislocated according to the orthopedist. However, in this group, when the emergency physician was sure of the joint condition, there was no significant difference between the opinion of the physician and the orthopedist [15-17].
On the other hand, 8 fractures were seen in group 2, which was a significant number of cases with dislocation-fracture in patients with unsuccessful reduction or uncertainty of joint condition after reduction. The physician's diagnostic accuracy was significantly lower than the reduction status in these individuals. There was a significant difference between the opinion of the physician and the orthopedist, so in cases with fractures, radiography should be performed after reduction because in these cases, it is difficult to assess the condition of the joint with examination [19, 20].
In group 2 patients whose radiographs did not have fractures, we again saw very high diagnostic accuracy of physicians at full confidence (100%); There was no significant difference between the opinion of the physician and the orthopedist. Therefore, we conclude that in cases of first shoulder dislocation or by impact mechanism, if no fracture is seen in pre-reduction radiography, post-reduction radiography can be removed if the physician is sure of complete reduction [21-23].
Today, doctors routinely request radiographs of the shoulder before and after reduction of the anterior shoulder dislocation. Performing radiography before and after anterior shoulder reduction is one of the topics discussed by orthopedic and emergency medicine specialists. A group of researchers believe that this dislocation can be easily detected by taking a history and detailed examination. Other studies, on the other hand, have questioned post-reduction radiography. In these studies, reducing pain, hearing reduction clicks, and improving range of motion of the joint instead of radiographs have been recommended [23-26].
The percentage of reduction in shoulder dislocation, regardless of the type of reduction technique, is 70 to 96%. The reduction success rate in this study was 94%. In two studies performed on 69 and 104 patients, 2 and 5 reduction failures occurred, respectively. This was 7 cases in our study, which may be due to age and physical differences of patients or due to greater caution and consideration, in order not to cause secondary damage during reduction in our study. In the two studies, no significant new fractures were seen following reduction, which is consistent with the results of the present study [27-29].
Several researchers have studied the need for radiography before and after shoulder dislocation reduction. These doctors developed an algorithm for the need for radiography. According to this algorithm, the radiograph of the shoulder in the case of the first dislocation, cases with trauma and uncertainty of the doctor of the joint position were taken. With this algorithm, a 46% reduction in radiographs and significant time savings were observed. On the other hand, no case of fracture or missing dislocation was found in cases without shoulder radiography (by telephone follow-up). Finally, the researchers concluded that the physician's opinion in determining the location of the humerus is very accurate, so in case of shoulder dislocation, radiography should be requested selectively and according to the recommended algorithm [29-31].
Another study on postoperative radiographic value was performed on 73 patients with anterior shoulder dislocation. In this study, about 37% of fractures were seen only in post-reduction radiography, however, none of these missed fractures interfered with the treatment of dislocation. The researchers concluded that anterior shoulder dislocations may be associated with fractures that are not seen on primary radiography due to the small size or position of the joint, but these fractures do not change the patient's healing process [31].
This study has some limitations. A number of eligible patients may not be included in the study due to lack of diagnosis by the physician (false negative), physicians' skills in examining the shoulder joint vary, and on the other hand, a number of small fractures may not be seen on radiography.
Conclusion
Physicians are able to accurately diagnose dislocation and reduction in cases of non-fracture shoulder dislocations. Shoulder radiography should be requested at a time when the physician is unsure of the condition of the joint. In the first dislocation or with the mechanism of radiographic shock should be done before reduction. In these patients, postoperative radiography should be limited to cases with fractures or suspected. Therefore, when the physician determines the condition of the shoulder joint through examination and history, shoulder radiography does not add a new point that changes the patient's treatment process.
Acknowledgements: None declared by the authors.
Ethical Permission: This study was performed after approval by the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.1250).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
References
1. Eljabu W, Klinger HM, von Knoch M. The natural course of shoulder instability and treatment trends: A systematic review. J Orthop Traumatol. 2017;18(1):1-8. [Link] [DOI:10.1007/s10195-016-0424-9]
2. Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V. Management of primary acute anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy. 2014;30(4):506-22. [Link] [DOI:10.1016/j.arthro.2014.01.003]
3. Helfen T, Ockert B, Pozder P, Regauer M, Haasters F. Management of prehospital shoulder dislocation: Feasibility and need of reduction. Eur J Trauma Emerg Surg. 2016;42(3):357-62 [Link] [DOI:10.1007/s00068-015-0545-5]
4. Siebenbürger G, Zeckey C, Fürmetz J, Ockert B, Böcker W, Helfen T. Medical speciality, medication or skills: Key factors of prehospital joint reduction: A prospective, multicenter cohort study. Eur J Trauma Emerg Surg. 2014;44(4):637-42. [Link] [DOI:10.1007/s00068-018-0933-8]
5. Bokor-Billmann T, Lapshyn H, Kiffner E, Goos MF, Hopt UT, Billmann FG. Reduction of acute shoulder dislocations in a remote environment: A prospective multicenter observational study. Wilderness Environ Med. 2015;26(3):395-400. [Link] [DOI:10.1016/j.wem.2014.12.027]
6. Lebus GF, Raynor MB, Nwosu SK, Wagstrom E, Jani SS, Carey JL, et al. Predictors for Surgery in shoulder instability: A retrospective cohort study using the FEDS system. Orthop J Sports Med. 2015;3(10):2325967115607434. [Link] [DOI:10.1177/2325967115607434]
7. Kanji A, Atkinson P, Fraser J, Lewis D, Benjamin S. Delays to initial reduction attempt are associated with higher failure rates in anterior shoulder dislocation: A retrospective analysis of factors affecting reduction failure. Emerg Med J. 2016;33(2):130-3. [Link] [DOI:10.1136/emermed-2015-204746]
8. Tajima K, Nishida Y, Shimizu C, Hori S. Double traction method-an easy and safe reduction method for anterior shoulder dislocations, even for non-orthopedic surgeons. Acute Med Surg. 2015;3(3):272-5. [Link] [DOI:10.1002/ams2.179]
9. Olivos-Meza A, Almazán-Diaz A, Calvo JA, Jiménez-Aroche CA, Valdez-Chávez MV, Pérez-Jiménez F, et al. Radiographic displacement of acute acromioclavicular joint dislocations fixed with AC tightrope. JSES Int. 2020;4(1):49-54. [Link] [DOI:10.1016/j.jseint.2019.11.002]
10. Cano-Martínez JA, Nicolás-Serrano G, Bento-Gerard J, Picazo-Marín F, Andrés-Grau J. Acute high-grade acromioclavicular dislocations treated with triple button device (MINAR): Preliminary results. Injury. 2016;47(11):2512-9. [Link] [DOI:10.1016/j.injury.2016.09.029]
11. Faria RS, Ribeiro FR, Amin BO, Junior AC, Costa MP, Filho CS, et al. Acromioclavicular dislocation: Postoperative evaluation of the coracoclavicular ligaments using magnetic resonance. Rev Bras Ortop. 2015;50(2):195-9. [Link] [DOI:10.1016/j.rboe.2015.04.007]
12. Weiser L, Nüchtern JV, Sellenschloh K, Püschel K, Morlock MM, Rueger JM, et al. Acromioclavicular joint dislocations: Coracoclavicular reconstruction with and without additional direct acromioclavicular repair. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2025-31. [Link] [DOI:10.1007/s00167-015-3920-1]
13. Vulliet P, Le Hanneur M, Cladiere V, Loriaut P, Boyer P. A comparison between two double-button endoscopically assisted surgical techniques for the treatment acute acromioclavicular dislocations. Musculoskelet Surg. 2018;102(1):73-9. [Link] [DOI:10.1007/s12306-017-0501-0]
14. Schliemann B, Roblenbroich SB, Schneider KN, Theisen C, Petersen W, Raschke MJ, Weimann A. Why does minimally invasive coracoclavicular ligament reconstruction using a flip button repair technique fail? An analysis of risk factors and complications. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1419-25. [Link] [DOI:10.1007/s00167-013-2737-z]
15. Di Giacomo GD, Golijanin P, Sanchez G, Provencher MT. Radiographic analysis of the hill-sachs lesion in anteroinferior shoulder instability after first-time dislocations. Arthroscopy. 2016;32(8):1509-14. [Link] [DOI:10.1016/j.arthro.2016.01.022]
16. Fox JA, Sanchez A, Zajac TJ, Provencher MT. Understanding the hill-sachs lesion in its role in patients with recurrent anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10(4):469-79. [Link] [DOI:10.1007/s12178-017-9437-0]
17. Saqib R, Harris J, Funk L. Comparison of magnetic resonance arthrography with arthroscopy for imaging of shoulder injuries: Retrospective study. Ann R Coll Surg Engl. 2017;99(4):271-4. [Link] [DOI:10.1308/rcsann.2016.0249]
18. Berg BV, Omoumi P. Dislocation of the shoulder joint-radiographic analysis of osseous abnormalities. J Belg Soc Radiol. 2016;100(1):89. [Link] [DOI:10.5334/jbr-btr.1210]
19. Lädermann A, Denard PJ, Boileau P, Farron A, Deransart P, Terrier A, et al. Effect of humeral stem design on humeral position and range of motion in reverse shoulder arthroplasty. Int Orthop. 2015;39(11):2205-13. [Link] [DOI:10.1007/s00264-015-2984-3]
20. Cusick MC, Hussey MM, Steen BM, Hartzler RU, Clark RE, Cuff DJ, et al. Glenosphere dissociation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(7):1061-8. [Link] [DOI:10.1016/j.jse.2014.12.019]
21. Lópiz Y, Rodríguez-González A, García-Fernández C, Marco F. Scapula insufficiency fractures after reverse total shoulder arthroplasty in rotator cuff arthropathy: What is their functional impact?. Rev Esp Cir Ortop Traumatol. 2015;59(5):318-25. [Link] [DOI:10.1016/j.recote.2015.07.007]
22. Mayne IP, Bell SN, Wright W, Coghlan JA. Acromial and scapular spine fractures after reverse total shoulder arthroplasty. Shoulder Elbow. 2016;8(2):90-100. [Link] [DOI:10.1177/1758573216628783]
23. Kennon JC, Lu C, McGee-Lawrence ME, Crosby LA. Scapula fracture incidence in reverse total shoulder arthroplasty using screws above or below metaglene central cage: Clinical and biomechanical outcomes. J Shoulder Elbow Surg. 2017;26(6):1023-30. [Link] [DOI:10.1016/j.jse.2016.10.018]
24. Ascione F, Kilian CM, Laughlin MS, Bugelli G, Domos P, Neyton L. Increased scapular spine fractures after reverse shoulder arthroplasty with a humeral onlay short stem: an analysis of 485 consecutive cases. J Shoulder Elbow Surg. 2018;27(12):2183-90. [Link] [DOI:10.1016/j.jse.2018.06.007]
25. King JJ, Dalton SS, Gulotta LV, Wright TW, Schoch BS. How common are acromial and scapular spine fractures after reverse shoulder arthroplasty?: A systematic review. Bone Joint J. 2019;101-B(6):627-34. [Link] [DOI:10.1302/0301-620X.101B6.BJJ-2018-1187.R1]
26. Neyton L, Erickson J, Ascione F, Bugelli G, Lunini E, Walch G. Grammont award 2018: Scapular fractures in reverse shoulder arthroplasty (Grammont style): Prevalence, functional, and radiographic results with minimum 5-year follow-up. J Shoulder Elbow Surg. 2019;28(2):260-7. [Link] [DOI:10.1016/j.jse.2018.07.004]
27. Schenk P, Aichmair A, Beeler S, Ernstbrunner L, Meyer DC, Gerber C. Acromial fractures following reverse total shoulder arthroplasty: A cohort-controlled analysis. Orthopedics. 2020;43(1):15-22. [Link] [DOI:10.3928/01477447-20191031-03]
28. Kerrigan AM, Reeves JM, Langohr GD, Johnson JA, Athwal GS. The influence of reverse arthroplasty humeral component design features on scapular spine strain. J Shoulder Elbow Surg. 2021;30(3):572-9. [Link] [DOI:10.1016/j.jse.2020.06.011]
29. Taylor SA, Shah SS, Chen X, Gentile J, Gulotta LV, Dines JS. Scapular ring preservation: coracoacromial ligament transection increases scapular spine strains following reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2020;102(15):1358-64. [Link] [DOI:10.2106/JBJS.19.01118]
30. Cho CH, Jung JW, Na SS, Bae KC, Lee KJ, Kim DH. Is acromial fracture after reverse total shoulder arthroplasty a negligible complication?: A systematic review. Clin Orthop Surg. 2019;11(4):427-35. [Link] [DOI:10.4055/cios.2019.11.4.427]
31. Lau SC, Large R. Acromial fracture after reverse total shoulder arthroplasty: A systematic review. Shoulder Elbow. 2020;12(6):375-89. [Link] [DOI:10.1177/1758573219876486]