GMJ Medicine
eISSN : 2626-3041
Volume 2, Issue 2 (2023)
GMJM 2023, 2(2): 63-66 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/11/4 | Accepted: 2023/03/10 | Published: 2023/05/7
Received: 2022/11/4 | Accepted: 2023/03/10 | Published: 2023/05/7
How to cite this article
Saboktakin L. Comparison of Systolic and Diastolic Blood Pressure Between Obese and Normal Weight Children. GMJM 2023; 2 (2) :63-66
URL: http://gmedicine.de/article-2-191-en.html
URL: http://gmedicine.de/article-2-191-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
L. Saboktakin *
“Tuberculosis and Lung Disease Research Center” and “Department of Otorhinolaryngology”, Tabriz University of medical Sciences, Tabriz, Iran
Keywords:
| Abstract (HTML) (1500 Views)
Full-Text: (578 Views)
Introduction
A child with high blood pressure will have many problems in adulthood if not treated in the same child. High blood pressure is a relatively dangerous disease, as long as it is not controlled. High blood pressure is often caused by poor nutrition, stress and sedentary lifestyle, but in some cases, high blood pressure can be inherited [1, 2].
Hypertension or so-called hypertension is not common in children and adolescents compared to adults, but if there is a sign of a serious and underlying disease such as kidney disease, heart disease or endocrine and .... In order to diagnose and treat hypertension early in children and adolescents, it should be measured in all children over 3 years of age, especially in cases with a family history of hypertension [3]. Accurate measurement of blood pressure, in addition to the doctor's attention and attention, also depends on the comfort and convenience of the child. Patients in Herseni, if they experience anxiety or worry when their blood pressure is measured, their blood pressure will rise falsely. For this purpose, the child can be placed on the parent's feet and their pressure can be measured [4].
These children may be slightly obese, but other symptoms, if present, include headache, dizziness, nosebleeds, anorexia, vision changes, and seizures. In cases of high blood pressure, kidney disease may cause growth failure [5].
Because genetics is also an important and powerful factor in blood pressure, in cases where the adolescent is in adolescence and his blood pressure is slightly higher than normal and his relatives have high blood pressure, blood pressure should be measured over the next few months [6, 7]. Regularly measured and controlled. The first and most essential principle of treatment, as well as prevention, is the control of the child's weight and treatment of obesity, which in cases of mild hypertension, treatment of obesity can cause a slight decrease in blood pressure, as well as having a regular exercise program, reducing salt intake and Fat is essential.
Considering that in the last decade, obesity in children has been increasing significantly and obesity is directly related to high blood pressure, we decided to examine the status of blood pressure in terms of body mass index in children under 15 years.
Instrument and Methods
Study design
This study was a cross-sectional descriptive study that was conducted during 2018 and 2019 in the health centers of Tabriz with the participation of 1000 under 9-year-old children. Taking into account the study sensitivity of 15%, alpha of 0.05 and reading power of 80%, the sample size was estimated to be 500 people, which to increase the study power, the number of samples was doubled. Sampling method was available in this study.
Inclusion and exclusion criteria
Inclusion criteria were age less than 9 years, gender of girls and boys and consent to participate in the study. Exclusion criteria included developmental disorders, endocrine disorders, and mental illness.
Procedure
Demographic characteristics of study participants such as age and sex, height, weight and body mass index were measured. Body mass index (BMI) is obtained by dividing weight (kg) by square height (meters). BMI does not directly measure the amount of body fat, but rather the amount of body fat compared to bone and muscle tissue. The result of calculating body mass index determines whether a person is obese, overweight, normal or very thin. In general, because BMI is easier and more effective than other methods of calculating proper weight, it is used almost all over the world as a basis for measuring body mass. The formula for calculating body fat mass is as follows. Based on this, individuals were divided into the following categories: severe underweight, underweight, normal weight, overweight, class 1 obesity, class 2 obesity and class 3 obesity. Then, the blood pressure of all children was measured while sitting and 10 minutes away from the children's right hand.
Ethical considerations
After coordination with the Vice Chancellor for Health of Tabriz University of Medical Sciences and explaining the goals in simple language to the participants, sampling began. Participants did not pay any fees for participating in this study.
Statistical analysis
The data were entered into the SPSS 21 software, using frequency, percentage, mean and standard deviation to display the data. T-test was used to compare between the two groups. ANOVA statistical test was also used for group comparison.
Findings
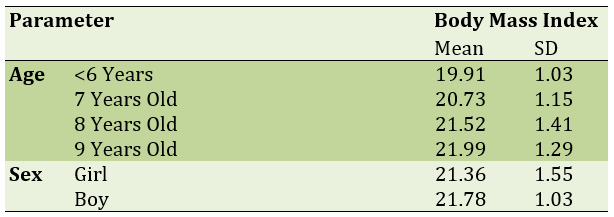
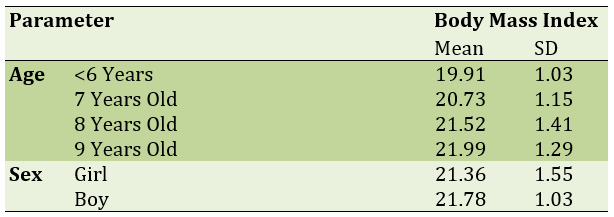
The mean age of study participants was 7.41±1.29 years; There was no statistically significant difference between the mean age of girls (7.27±1.14) and boys (7.71±1.41) participating in the study (p=0.598). The mean body mass index in all study participants was 21.41±2.16 (Table 1).
The mean total systolic blood pressure of the study participants was 101.49±6.18 and the mean total diastolic blood pressure of the study participants was 65.19±4.12. Comparison of mean systolic blood pressure in boys (100.41±11.96) and girls (102.85±12.19) participating in the study was statistically significant; Also, the comparison of mean diastolic blood pressure in boys (63.49±4.02) and girls (65.01±4.59) in the study was not statistically significant.
Table 1) Body mass index by age and gender in study participants
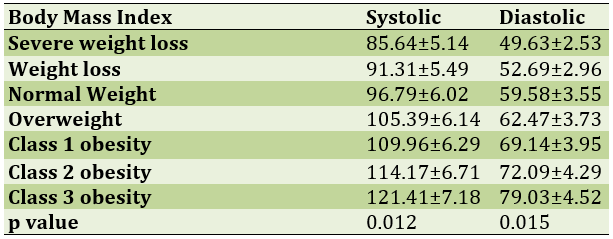
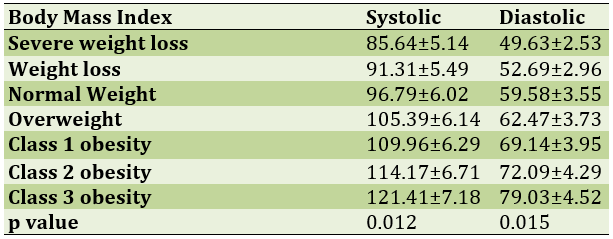
Examination of systolic and diastolic blood pressure based on body mass index showed that with increasing body mass index, blood pressure was significantly increased. In other words, obesity and overweight as a risk factor for high blood pressure (Table 2).
Table 2) Comparison of systolic and diastolic blood pressure changes based on body mass index classification
Discussion
Blood pressure refers to the force that blood exerts on the walls of the body as it passes through the arteries. Under normal circumstances, the heart pumps blood into arteries throughout the body [8]. The arteries dilate and contract as needed to keep blood flowing smoothly. High blood pressure is a condition in which the force on the walls of the arteries is much greater than normal. In a person with high blood pressure, at any age, the blood presses too hard on the walls of the arteries, which The problem can damage the walls of blood vessels, the heart and other organs. Like adults, high blood pressure in children can have serious and long-term effects on their health. Adverse effects of high blood pressure in children include: heart disease, kidney disease, the possibility of stroke [9, 10]. The minimum blood pressure in infancy and at the age of 1 to 12 months is 70 over 50 and the normal blood pressure in this period is 90 over 60 and the maximum blood pressure in this period is 110 over 75 [11]. Gradually with age and entering the stage of childhood. And at the age of 1 to 5, the minimum pressure reaches about 80 over 55. Normal blood pressure during this period is 95 over 65 and if the blood pressure at this age is 110 over 79 it is very dangerous. Normal blood pressure at the age of 6 to 13 is 105 over 70 and the minimum pressure is 90 over 60 and the maximum is 115 zinc [12, 13].
Blood pressure in children and adolescents is a growing health problem that is often overlooked. If there are risk factors, children should be monitored annually for good blood pressure under the supervision of a good cardiologist. Normal blood pressure is 12 over 8. Blood pressure in children under 6 years of age is usually caused by another medical condition. Older children can develop high blood pressure for the same reasons that adults can develop high blood pressure - being overweight, malnourished and not exercising [14, 15]. Outpatient blood pressure monitoring should be performed to confirm hypertension in children and adolescents. Also, to evaluate underlying medical disorders, a history and physical examination and targeted screening tests should be performed and related diseases such as diabetes and hyperlipidemia should be evaluated. Hypertension in children is initially treated with lifestyle changes such as weight loss in case of overweight or obesity, healthy diet and regular exercise [16, 17]. Risk factors for high blood pressure in children include obesity and a family history of high blood pressure. Other risk factors may include medical problems such as hormonal abnormalities, congenital aortic stenosis, sleep apnea, or other sleep disorders. Obesity is considered to be the leading cause of high blood pressure in children. Obesity not only exposes your baby to high blood pressure, but also sets the stage for a range of other health problems, such as heart disease and diabetes [18, 19].
Lack of nutritional status, lack of stress control when measuring blood pressure and lack of accurate information about the amount of physical activity in children in the few hours before measuring blood pressure were the limitations of this study. It is recommended that more detailed studies be conducted in the future to address these limitations.
Conclusion
Obesity and weight gain is one of the main causes and risk factors for high blood pressure; In this study, it was observed that the higher the body mass index of children, the higher the systolic and diastolic blood pressure; In other words, high body mass index is an effective and strong risk factor in increasing blood pressure in children.
Acknowledgements: None declared by the authors.
Ethical Permission: This study was conducted after approval by the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.740).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
A child with high blood pressure will have many problems in adulthood if not treated in the same child. High blood pressure is a relatively dangerous disease, as long as it is not controlled. High blood pressure is often caused by poor nutrition, stress and sedentary lifestyle, but in some cases, high blood pressure can be inherited [1, 2].
Hypertension or so-called hypertension is not common in children and adolescents compared to adults, but if there is a sign of a serious and underlying disease such as kidney disease, heart disease or endocrine and .... In order to diagnose and treat hypertension early in children and adolescents, it should be measured in all children over 3 years of age, especially in cases with a family history of hypertension [3]. Accurate measurement of blood pressure, in addition to the doctor's attention and attention, also depends on the comfort and convenience of the child. Patients in Herseni, if they experience anxiety or worry when their blood pressure is measured, their blood pressure will rise falsely. For this purpose, the child can be placed on the parent's feet and their pressure can be measured [4].
These children may be slightly obese, but other symptoms, if present, include headache, dizziness, nosebleeds, anorexia, vision changes, and seizures. In cases of high blood pressure, kidney disease may cause growth failure [5].
Because genetics is also an important and powerful factor in blood pressure, in cases where the adolescent is in adolescence and his blood pressure is slightly higher than normal and his relatives have high blood pressure, blood pressure should be measured over the next few months [6, 7]. Regularly measured and controlled. The first and most essential principle of treatment, as well as prevention, is the control of the child's weight and treatment of obesity, which in cases of mild hypertension, treatment of obesity can cause a slight decrease in blood pressure, as well as having a regular exercise program, reducing salt intake and Fat is essential.
Considering that in the last decade, obesity in children has been increasing significantly and obesity is directly related to high blood pressure, we decided to examine the status of blood pressure in terms of body mass index in children under 15 years.
Instrument and Methods
Study design
This study was a cross-sectional descriptive study that was conducted during 2018 and 2019 in the health centers of Tabriz with the participation of 1000 under 9-year-old children. Taking into account the study sensitivity of 15%, alpha of 0.05 and reading power of 80%, the sample size was estimated to be 500 people, which to increase the study power, the number of samples was doubled. Sampling method was available in this study.
Inclusion and exclusion criteria
Inclusion criteria were age less than 9 years, gender of girls and boys and consent to participate in the study. Exclusion criteria included developmental disorders, endocrine disorders, and mental illness.
Procedure
Demographic characteristics of study participants such as age and sex, height, weight and body mass index were measured. Body mass index (BMI) is obtained by dividing weight (kg) by square height (meters). BMI does not directly measure the amount of body fat, but rather the amount of body fat compared to bone and muscle tissue. The result of calculating body mass index determines whether a person is obese, overweight, normal or very thin. In general, because BMI is easier and more effective than other methods of calculating proper weight, it is used almost all over the world as a basis for measuring body mass. The formula for calculating body fat mass is as follows. Based on this, individuals were divided into the following categories: severe underweight, underweight, normal weight, overweight, class 1 obesity, class 2 obesity and class 3 obesity. Then, the blood pressure of all children was measured while sitting and 10 minutes away from the children's right hand.
Ethical considerations
After coordination with the Vice Chancellor for Health of Tabriz University of Medical Sciences and explaining the goals in simple language to the participants, sampling began. Participants did not pay any fees for participating in this study.
Statistical analysis
The data were entered into the SPSS 21 software, using frequency, percentage, mean and standard deviation to display the data. T-test was used to compare between the two groups. ANOVA statistical test was also used for group comparison.
Findings
The mean age of study participants was 7.41±1.29 years; There was no statistically significant difference between the mean age of girls (7.27±1.14) and boys (7.71±1.41) participating in the study (p=0.598). The mean body mass index in all study participants was 21.41±2.16 (Table 1).
The mean total systolic blood pressure of the study participants was 101.49±6.18 and the mean total diastolic blood pressure of the study participants was 65.19±4.12. Comparison of mean systolic blood pressure in boys (100.41±11.96) and girls (102.85±12.19) participating in the study was statistically significant; Also, the comparison of mean diastolic blood pressure in boys (63.49±4.02) and girls (65.01±4.59) in the study was not statistically significant.
Table 1) Body mass index by age and gender in study participants
Examination of systolic and diastolic blood pressure based on body mass index showed that with increasing body mass index, blood pressure was significantly increased. In other words, obesity and overweight as a risk factor for high blood pressure (Table 2).
Table 2) Comparison of systolic and diastolic blood pressure changes based on body mass index classification
Discussion
Blood pressure refers to the force that blood exerts on the walls of the body as it passes through the arteries. Under normal circumstances, the heart pumps blood into arteries throughout the body [8]. The arteries dilate and contract as needed to keep blood flowing smoothly. High blood pressure is a condition in which the force on the walls of the arteries is much greater than normal. In a person with high blood pressure, at any age, the blood presses too hard on the walls of the arteries, which The problem can damage the walls of blood vessels, the heart and other organs. Like adults, high blood pressure in children can have serious and long-term effects on their health. Adverse effects of high blood pressure in children include: heart disease, kidney disease, the possibility of stroke [9, 10]. The minimum blood pressure in infancy and at the age of 1 to 12 months is 70 over 50 and the normal blood pressure in this period is 90 over 60 and the maximum blood pressure in this period is 110 over 75 [11]. Gradually with age and entering the stage of childhood. And at the age of 1 to 5, the minimum pressure reaches about 80 over 55. Normal blood pressure during this period is 95 over 65 and if the blood pressure at this age is 110 over 79 it is very dangerous. Normal blood pressure at the age of 6 to 13 is 105 over 70 and the minimum pressure is 90 over 60 and the maximum is 115 zinc [12, 13].
Blood pressure in children and adolescents is a growing health problem that is often overlooked. If there are risk factors, children should be monitored annually for good blood pressure under the supervision of a good cardiologist. Normal blood pressure is 12 over 8. Blood pressure in children under 6 years of age is usually caused by another medical condition. Older children can develop high blood pressure for the same reasons that adults can develop high blood pressure - being overweight, malnourished and not exercising [14, 15]. Outpatient blood pressure monitoring should be performed to confirm hypertension in children and adolescents. Also, to evaluate underlying medical disorders, a history and physical examination and targeted screening tests should be performed and related diseases such as diabetes and hyperlipidemia should be evaluated. Hypertension in children is initially treated with lifestyle changes such as weight loss in case of overweight or obesity, healthy diet and regular exercise [16, 17]. Risk factors for high blood pressure in children include obesity and a family history of high blood pressure. Other risk factors may include medical problems such as hormonal abnormalities, congenital aortic stenosis, sleep apnea, or other sleep disorders. Obesity is considered to be the leading cause of high blood pressure in children. Obesity not only exposes your baby to high blood pressure, but also sets the stage for a range of other health problems, such as heart disease and diabetes [18, 19].
Lack of nutritional status, lack of stress control when measuring blood pressure and lack of accurate information about the amount of physical activity in children in the few hours before measuring blood pressure were the limitations of this study. It is recommended that more detailed studies be conducted in the future to address these limitations.
Conclusion
Obesity and weight gain is one of the main causes and risk factors for high blood pressure; In this study, it was observed that the higher the body mass index of children, the higher the systolic and diastolic blood pressure; In other words, high body mass index is an effective and strong risk factor in increasing blood pressure in children.
Acknowledgements: None declared by the authors.
Ethical Permission: This study was conducted after approval by the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.740).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
References
1. Roulet C, Bovet P, Brauchli T, Simeoni U, Xi B, Santschi V, et al. Secular trends in blood pressure in children: A systematic review. J Clin Hypertens (Greenwich). 2017;19(5):488-97. [Link] [DOI:10.1111/jch.12955]
2. Noubiap JJ, Essouma M, Bigna JJ, Jingi AM, Aminde LN, Nansseu JR. Prevalence of elevated blood pressure in children and adolescents in Africa: A systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e375-86. [Link] [DOI:10.1016/S2468-2667(17)30123-8]
3. Högström G, Nordström A, Eriksson M, Nordström P. Risk factors assessed in adolescence and the later risk of stroke in men: A 33-year follow-up study. Cerebrovasc Dis. 2015;39(1):63-71. [Link] [DOI:10.1159/000369960]
4. Xi B, Zhang T, Li S, Harville E, Bazzano L, He J, Chen W. Can pediatric hypertension criteria be simplified? A prediction analysis of subclinical cardiovascular outcomes from the Bogalusa Heart Study. Hypertension. Hypertension. 2017;69(4):691-6. [Link] [DOI:10.1161/HYPERTENSIONAHA.116.08782]
5. Yan Y, Hou D, Liu J, Zhao X, Cheng H, Xi B, et al. Childhood body mass index and blood pressure in prediction of subclinical vascular damage in adulthood: Beijing blood pressure cohort. J Hypertens. 2017;35(1):47-54. [Link] [DOI:10.1097/HJH.0000000000001118]
6. Koskinen J, Juonala M, Dwyer T, Venn A, Thomson R, Bazzano L, et al. Impact of lipid measurements in youth in addition to conventional clinic-based risk factors on predicting preclinical atherosc. Circulation. 2018;137(12):1246-55. [Link] [DOI:10.1161/CIRCULATIONAHA.117.029726]
7. Koskinen J, Juonala M, Dwyer T, Venn A, Petkeviciene J, Čeponienė I, et al. Utility of different blood pressure measurement components in childhood to predict adult carotid intima-media thickness. Hyper. 2019;73(2):335-41. [Link] [DOI:10.1161/HYPERTENSIONAHA.118.12225]
8. Du T, Fernandez C, Barshop R, Chen W, Urbina EM, Bazzano LA. 2017 Pediatric hypertension guidelines improve prediction of adult cardiovascular outcomes. Hyper. 2019;73(6):1217-23. [Link] [DOI:10.1161/HYPERTENSIONAHA.118.12469]
9. Yan Y, Liu J, Wang L, Hou D, Zhao X, Cheng H, et al. Independent influences of excessive body weight and elevated blood pressure from childhood on left ventricular geometric remodeling in adulthood. Int J Cardiol. 2017;243:492-6. [Link] [DOI:10.1016/j.ijcard.2017.05.085]
10. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904. [Link] [DOI:10.1542/peds.2017-3035]
11. Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, et al. 2016 European society of hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34(10):1887-920. [Link] [DOI:10.1097/HJH.0000000000001039]
12. Magnussen CG, Smith KJ. Pediatric blood pressure and adult preclinical markers of cardiovascular disease. Clin Med Insights Blood Disord. 2016;9:CMBD-S18887. [Link] [DOI:10.4137/CMBD.S18887]
13. Leiba A, Twig G, Levine H, Goldberger N, Afek A, Shamiss A, et al. Hypertension in late adolescence and cardiovascular mortality in midlife: A cohort study of 2.3 million 16-to 19-year-old examinees. Pediatr Nephrol. 2016;31(3):485-92. [Link] [DOI:10.1007/s00467-015-3240-1]
14. Aatola H, Koivistoinen T, Tuominen H, Juonala M, Lehtimäki T, Viikari JS, et al. Influence of child and adult elevated blood pressure on adult arterial stiffness: The cardiovascular risk in young finns study. Hypertension. 2017;70(3):531-6. [Link] [DOI:10.1161/HYPERTENSIONAHA.117.09444]
15. Berenson GS, Srinivasan SR, Xu HJ, Chen W. Adiposity and cardiovascular risk factor variables in childhood are associated with premature death from coronary heart disease in adults: The bogalusa heart study. Am J Med Sci. 2016;352(5):448-54. [Link] [DOI:10.1016/j.amjms.2016.08.006]
16. Yano Y, Reis JP, Colangelo LA, Shimbo D, Viera AJ, Allen NB, et al. Association of blood pressure classification in young adults using the 2017 American college of cardiology/American heart association blood pressure guideline with cardiovascular events later in life. JAMA. 2018;320(17):1774-82. [Link] [DOI:10.1001/jama.2018.13551]
17. Son JS, Choi S, Kim K, Kim M, Choi D, Lee G, et al. Association of blood pressure classification in Korean young adults according to the 2017 American college of cardiology/American heart association guidelines with subsequent cardiovascular disease events. JAMA. 2018;320(17):1783-92. [Link] [DOI:10.1001/jama.2018.16501]
18. Briasoulis A, Androulakis E, Palla M, Papageorgiou N, Tousoulis D. White-coat hypertension and cardiovascular events: a meta-analysis. J Hypertens. 2016;34(4):593-9. [Link] [DOI:10.1097/HJH.0000000000000832]
19. Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. 2018;2(3):223-8. [Link] [DOI:10.1016/S2352-4642(18)30022-1]









