GMJ Medicine
eISSN : 2626-3041
Volume 2, Issue 1 (2023)
GMJM 2023, 2(1): 35-38 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/07/12 | Accepted: 2022/11/27 | Published: 2023/01/22
Received: 2022/07/12 | Accepted: 2022/11/27 | Published: 2023/01/22
How to cite this article
Mohammadipour Anvari H, Sadeghi S. Relationship Between Serum CRP Levels and Mortality; one Year After Coronary Artery Bypass Graft Surgery. GMJM 2023; 2 (1) :35-38
URL: http://gmedicine.de/article-2-194-en.html
URL: http://gmedicine.de/article-2-194-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
H. Mohammadipour Anvari *1, S. Sadeghi1
1- Tuberculosis and Lung Disease Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Keywords:
| Abstract (HTML) (1611 Views)
Full-Text: (481 Views)
Introduction
In of the most important and common diseases that are increasingly seen in developed and developing countries today is heart disease, led by acute myocardial infarction (AMI). Many patients with this disease suffer from side effects from minor cases to severe heart failure and mortality, so that the mortality rate due to acute stroke is reported to be about 30% due to the importance of this disease and its complications, various imaging methods including and serological tests are performed to diagnose the disease and determine its severity. Numerous factors also occur during this complication, the measurement of which can help determine the severity of inflammation and involvement of the heart muscle [1]. One of the most important factors is the study of acute phase reactive protein (CRP). This protein is of hepatic origin and its serum level in the plasma of different people can be measured in low amounts. It is also one of the factors of non-specific defense of the host against inflammation it is usually increased in inflammatory processes. Chronic inflammation is also an important component of vascular atherosclerosis and its severity is directly related to serum CRP levels. So far, this protein has been used as a marker in predicting risk in normal people and patients with angina [2].
Today, several studies have been performed to determine the relationship between this factor and the mortality rate of patients after coronary artery bypass graft surgery, which has sometimes been favorable in predicting short-term mortality (1 month) of these patients without conclusions [3, 4]. Therefore, the aim of this study was to determine the relationship between serum CRP levels before general anesthesia and one-month mortality in patients after coronary artery bypass graft surgery.
Instrument and Methods
This descriptive-analytical study was performed on patients after coronary artery bypass graft surgery who were admitted to the intensive care unit of Shahid Madani Hospital (Tabriz Medical Sciences) for one year. Patients with stable angina, unstable angina, had non-cardiac chest pain, and patients with malignancy, active mediastinal diseases, febrile sepsis, sepsis, and respiratory disease (COPD, bronchitis, pulmonary tuberculosis) were excluded.
Patients with chest pain and a diagnosis of AMI were admitted to a hospital CCU with a 2-4cc plasma sample taken after 24 hours and mixed with EDTA or heparin. It was then sent to the lab. Sometimes it was necessary to cool the patient's plasma sample to be sent, which could be stored at 2-8°C for up to 8 days and in case of Freeze at 20°C for up to 3 months. In this experiment, the CRP in the patient's sample complexes with polyclonal antibodies against CRP encoded on latex particles and creates turbidity. The amount of turbidity generated is directly related to the amount of CRP in the serum sample, which is by immunoturbidity amplified by measuring two points of photometer is obtained. The existing kit is of Pars test type and has a sensitivity between the values of 0.1mg/l and up to 20mg/l. Normal CRP value according to this kit is less in adults. Patients were recorded and measured at 5mg/l CRP and then their mortality was assessed and followed up to 30 days after MI.
This study was performed after receiving the code (IR.TBZMED.REC.1399.980) of ethics from the ethics committee of Tabriz University of Medical Sciences. The available information was extracted from patients' files and finally the data were entered into SPSS software and the Regession method was used to analyze the information.
Findings
The mean age of patients in the deceased group was 73.2±8.6 years compared to the mean age of the non-deceased group (59.7±12.3 years), which indicates the presence of older people in the deceased group. With age, a higher percentage of patients have died, with the highest death rate in the 75 age group. It should be noted that none of the deaths in our study group were in the age group of less than 55 years. The most occupational groups are: disabled (44.7%) housewife (25.9%) and free, respectively (17.6%).
The presence of risk factors such as HTN, history of diabetes and smoking has significantly increased the mortality rate of our study group (p=0.002). So that the largest increase in mortality are: the presence of a history of hypertension in individuals and a history of smoking. Also, regular use of heart drugs in drug patients with a history of heart disease has reduced the mortality of these patients by about 11% (p=0.0001).
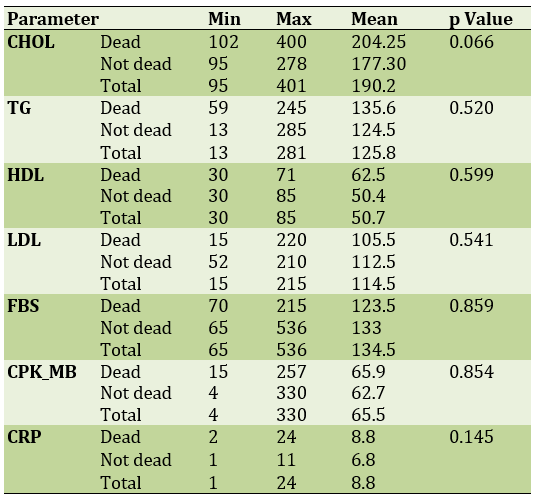
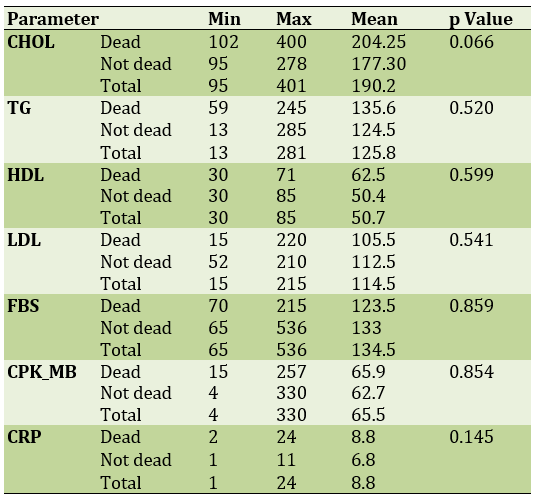
The difference between the fat and blood sugar elements is observed in the deceased and non-deceased groups, so that the most obvious difference is in the average cholesterol. Also, there is no significant difference in the mean HDL as a risk-reducing factor. In deceased patients, the mean hsCRP was 8.89 and higher than the mean hsCRP in the non-deceased group was 6.39 (p=0.146). Also, the mean CPKMB as a known cardiac marker in deceased patients increased slightly (p=0.851; Table 1).
In this study, 85 patients with acute myocardial infarction (AMI) were studied. In a one-month follow-up of these patients, 15 people died. In terms of sexual distribution, 41% of patients are female and 59% of them are male. Also, in examining the age distribution of these patients in the deceased and non-deceased groups, the mean age of the deceased was 73.2 years and the survivors were 59.7 years, respectively. As can be seen, the deceased had a higher average age (p= 0.0001). Most patients were in the age group of 75-65 years, as shown in Figure 2-4, the ratio of dead to live increases from the age of 65 years and the largest difference between The ratio of deaths to survivors is seen in the age group of years. And none of the patients who died were under the age of 45. Which can be justified due to the natural aging process and reduced response to acute inflammation. In the occupational study of our patients, the most common groups are: disabled (44.7%), housewife (26%) and free (17.6%). As can be seen, agricultural occupation, which is one of the heaviest jobs in terms of physical force use, has the lowest statistics (2.4%).
Table 1) Evaluation of the relationship between CRP and experimental results of patients with premature mortality
In the study of patients in terms of previous history and associated disorders, the presence of factors such as history of blood pressure (60% of patients died to 40% not died), history of diabetes mellitus (46% of deaths to 38% of patients not died) and history of smoking and smoking (60% of patients who died to 44 did not die) caused a significant increase in the deceased group compared to the non-deceased group (p=0.002). They have a higher risk of death and mortality than people without this record (73% of deaths versus 67% of non-deaths). Also, according to the results, a history of regular drug use reduces the percentage of deaths to death (66.7% compared to 77.1%). History of surgical treatment also increased the mortality rate in patients with AMI (p=0.003).
As you can see in Table 4-4, the average increase in mean cholesterol-triglyceride, LDL is seen in deceased patients compared to non-deceased individuals. The highest difference in fat elements is seen in cholesterol (mean in 204 deaths compared to 177 deaths average) (p=0.066) Also, a statistically significant difference in HDL and FBS levels in patients in the dead and living groups. The residue is not seen.
Also, a study has been performed on patients' preclinical findings, the results of which are as follows:
EKG findings: 80 patients (94%) had STElevation symptoms on their ECG strip, of which 13 (16%) died. In the study of infarction in patients, respectively: 43% infarction of the inferior region (infMI), 34% in the anterior region (ANT-MI) and 17% in the antroceptal region and about 5% of patients with extensive MI (Extensive MI) are observed. Due to the prevalence, the highest mortality occurred due to lower MI (9%). It should be noted that the most deadly MI was Extensive MI (50% of deaths in this type).
CXR findings: 75% of patients had normal CXR, 17% had cardiomegaly and 7% had pulmonary edema. The highest mortality occurred due to the prevalence in patients with normal CXR. (9%) The most fatal conditions were pulmonary edema (50%) and cardiomegaly (26%), respectively.
*Drug history findings: 17% of patients did not report any history of drug use, 15% of patients with a history of B blocker use and 8% in addition to B blocker, used ASA in addition to half of patients History of use of a set of B-blockers NSAIDS and ASA ACE-Inh.
In the study of patients for hsCRP, the mean hsCRP in the deceased group was 8.89mg/l and in the non-deceased group was 6.39mg/l. (p=0.146) which shows the relationship between hsCRP and one-month death in patients with AMI. Also according to Figure (4-8) in deceased patients 60% of people have high hsCRP (values of 5mg/l≤). In 45% of patients who did not die, only those with high hsCRP levels. Which suggests the role of hsCRP in the relative determination of the short-term (one month) prognosis of patients with acute myocardial infarction.
As we know, there are several methods such as multiple imaging (echocardiography, CT angiography, MR angiography, etc.) to determine the degree of coronary artery involvement to determine the status of ischemia and myocardial infarction, which is very costly and time consuming. The aim of this study was to use an inexpensive and convenient serological method to estimate the overall framework of the patient's prognosis [5]. In a new study of a very large number of patients, the positive predictive value of hsCRP was higher, which highlights the importance of sample frequency in evaluating hsCRP as a predictive index. Also, according to previous studies on CRP (as an increasing factor in inflammatory activity) [6], this issue is of particular importance to identify comorbidities that have increased CRP in patients with acute myocardial infarction (AMI). To prevent false positives of hsCRP. There are many known diseases that increase hsCRP, such as rheumatic diseases, malignancies and lung diseases in patients with AMI (who are mostly elderly people in the community) [7, 8]. In this study, we tried to exclude all these patients. However, there may also be chronic undiagnosed inflammation that overlaps with the increase in hsCRP due to myocardial infarction [9-11].
Conclusion
The use of hsCRP should be combined with patient age, history of hypertension, history of smoking and history of diabetes mellitus. Although it seems that over time after an acute myocardial infarction, the value of hsCRP in determining the prognosis of death and mortality increases.
Acknowledgements: None declared by the authors.
Ethical Permission: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
In of the most important and common diseases that are increasingly seen in developed and developing countries today is heart disease, led by acute myocardial infarction (AMI). Many patients with this disease suffer from side effects from minor cases to severe heart failure and mortality, so that the mortality rate due to acute stroke is reported to be about 30% due to the importance of this disease and its complications, various imaging methods including and serological tests are performed to diagnose the disease and determine its severity. Numerous factors also occur during this complication, the measurement of which can help determine the severity of inflammation and involvement of the heart muscle [1]. One of the most important factors is the study of acute phase reactive protein (CRP). This protein is of hepatic origin and its serum level in the plasma of different people can be measured in low amounts. It is also one of the factors of non-specific defense of the host against inflammation it is usually increased in inflammatory processes. Chronic inflammation is also an important component of vascular atherosclerosis and its severity is directly related to serum CRP levels. So far, this protein has been used as a marker in predicting risk in normal people and patients with angina [2].
Today, several studies have been performed to determine the relationship between this factor and the mortality rate of patients after coronary artery bypass graft surgery, which has sometimes been favorable in predicting short-term mortality (1 month) of these patients without conclusions [3, 4]. Therefore, the aim of this study was to determine the relationship between serum CRP levels before general anesthesia and one-month mortality in patients after coronary artery bypass graft surgery.
Instrument and Methods
This descriptive-analytical study was performed on patients after coronary artery bypass graft surgery who were admitted to the intensive care unit of Shahid Madani Hospital (Tabriz Medical Sciences) for one year. Patients with stable angina, unstable angina, had non-cardiac chest pain, and patients with malignancy, active mediastinal diseases, febrile sepsis, sepsis, and respiratory disease (COPD, bronchitis, pulmonary tuberculosis) were excluded.
Patients with chest pain and a diagnosis of AMI were admitted to a hospital CCU with a 2-4cc plasma sample taken after 24 hours and mixed with EDTA or heparin. It was then sent to the lab. Sometimes it was necessary to cool the patient's plasma sample to be sent, which could be stored at 2-8°C for up to 8 days and in case of Freeze at 20°C for up to 3 months. In this experiment, the CRP in the patient's sample complexes with polyclonal antibodies against CRP encoded on latex particles and creates turbidity. The amount of turbidity generated is directly related to the amount of CRP in the serum sample, which is by immunoturbidity amplified by measuring two points of photometer is obtained. The existing kit is of Pars test type and has a sensitivity between the values of 0.1mg/l and up to 20mg/l. Normal CRP value according to this kit is less in adults. Patients were recorded and measured at 5mg/l CRP and then their mortality was assessed and followed up to 30 days after MI.
This study was performed after receiving the code (IR.TBZMED.REC.1399.980) of ethics from the ethics committee of Tabriz University of Medical Sciences. The available information was extracted from patients' files and finally the data were entered into SPSS software and the Regession method was used to analyze the information.
Findings
The mean age of patients in the deceased group was 73.2±8.6 years compared to the mean age of the non-deceased group (59.7±12.3 years), which indicates the presence of older people in the deceased group. With age, a higher percentage of patients have died, with the highest death rate in the 75 age group. It should be noted that none of the deaths in our study group were in the age group of less than 55 years. The most occupational groups are: disabled (44.7%) housewife (25.9%) and free, respectively (17.6%).
The presence of risk factors such as HTN, history of diabetes and smoking has significantly increased the mortality rate of our study group (p=0.002). So that the largest increase in mortality are: the presence of a history of hypertension in individuals and a history of smoking. Also, regular use of heart drugs in drug patients with a history of heart disease has reduced the mortality of these patients by about 11% (p=0.0001).
The difference between the fat and blood sugar elements is observed in the deceased and non-deceased groups, so that the most obvious difference is in the average cholesterol. Also, there is no significant difference in the mean HDL as a risk-reducing factor. In deceased patients, the mean hsCRP was 8.89 and higher than the mean hsCRP in the non-deceased group was 6.39 (p=0.146). Also, the mean CPKMB as a known cardiac marker in deceased patients increased slightly (p=0.851; Table 1).
In this study, 85 patients with acute myocardial infarction (AMI) were studied. In a one-month follow-up of these patients, 15 people died. In terms of sexual distribution, 41% of patients are female and 59% of them are male. Also, in examining the age distribution of these patients in the deceased and non-deceased groups, the mean age of the deceased was 73.2 years and the survivors were 59.7 years, respectively. As can be seen, the deceased had a higher average age (p= 0.0001). Most patients were in the age group of 75-65 years, as shown in Figure 2-4, the ratio of dead to live increases from the age of 65 years and the largest difference between The ratio of deaths to survivors is seen in the age group of years. And none of the patients who died were under the age of 45. Which can be justified due to the natural aging process and reduced response to acute inflammation. In the occupational study of our patients, the most common groups are: disabled (44.7%), housewife (26%) and free (17.6%). As can be seen, agricultural occupation, which is one of the heaviest jobs in terms of physical force use, has the lowest statistics (2.4%).
Table 1) Evaluation of the relationship between CRP and experimental results of patients with premature mortality
In the study of patients in terms of previous history and associated disorders, the presence of factors such as history of blood pressure (60% of patients died to 40% not died), history of diabetes mellitus (46% of deaths to 38% of patients not died) and history of smoking and smoking (60% of patients who died to 44 did not die) caused a significant increase in the deceased group compared to the non-deceased group (p=0.002). They have a higher risk of death and mortality than people without this record (73% of deaths versus 67% of non-deaths). Also, according to the results, a history of regular drug use reduces the percentage of deaths to death (66.7% compared to 77.1%). History of surgical treatment also increased the mortality rate in patients with AMI (p=0.003).
As you can see in Table 4-4, the average increase in mean cholesterol-triglyceride, LDL is seen in deceased patients compared to non-deceased individuals. The highest difference in fat elements is seen in cholesterol (mean in 204 deaths compared to 177 deaths average) (p=0.066) Also, a statistically significant difference in HDL and FBS levels in patients in the dead and living groups. The residue is not seen.
Also, a study has been performed on patients' preclinical findings, the results of which are as follows:
EKG findings: 80 patients (94%) had STElevation symptoms on their ECG strip, of which 13 (16%) died. In the study of infarction in patients, respectively: 43% infarction of the inferior region (infMI), 34% in the anterior region (ANT-MI) and 17% in the antroceptal region and about 5% of patients with extensive MI (Extensive MI) are observed. Due to the prevalence, the highest mortality occurred due to lower MI (9%). It should be noted that the most deadly MI was Extensive MI (50% of deaths in this type).
CXR findings: 75% of patients had normal CXR, 17% had cardiomegaly and 7% had pulmonary edema. The highest mortality occurred due to the prevalence in patients with normal CXR. (9%) The most fatal conditions were pulmonary edema (50%) and cardiomegaly (26%), respectively.
*Drug history findings: 17% of patients did not report any history of drug use, 15% of patients with a history of B blocker use and 8% in addition to B blocker, used ASA in addition to half of patients History of use of a set of B-blockers NSAIDS and ASA ACE-Inh.
In the study of patients for hsCRP, the mean hsCRP in the deceased group was 8.89mg/l and in the non-deceased group was 6.39mg/l. (p=0.146) which shows the relationship between hsCRP and one-month death in patients with AMI. Also according to Figure (4-8) in deceased patients 60% of people have high hsCRP (values of 5mg/l≤). In 45% of patients who did not die, only those with high hsCRP levels. Which suggests the role of hsCRP in the relative determination of the short-term (one month) prognosis of patients with acute myocardial infarction.
As we know, there are several methods such as multiple imaging (echocardiography, CT angiography, MR angiography, etc.) to determine the degree of coronary artery involvement to determine the status of ischemia and myocardial infarction, which is very costly and time consuming. The aim of this study was to use an inexpensive and convenient serological method to estimate the overall framework of the patient's prognosis [5]. In a new study of a very large number of patients, the positive predictive value of hsCRP was higher, which highlights the importance of sample frequency in evaluating hsCRP as a predictive index. Also, according to previous studies on CRP (as an increasing factor in inflammatory activity) [6], this issue is of particular importance to identify comorbidities that have increased CRP in patients with acute myocardial infarction (AMI). To prevent false positives of hsCRP. There are many known diseases that increase hsCRP, such as rheumatic diseases, malignancies and lung diseases in patients with AMI (who are mostly elderly people in the community) [7, 8]. In this study, we tried to exclude all these patients. However, there may also be chronic undiagnosed inflammation that overlaps with the increase in hsCRP due to myocardial infarction [9-11].
Conclusion
The use of hsCRP should be combined with patient age, history of hypertension, history of smoking and history of diabetes mellitus. Although it seems that over time after an acute myocardial infarction, the value of hsCRP in determining the prognosis of death and mortality increases.
Acknowledgements: None declared by the authors.
Ethical Permission: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
References
1. Aagaard T, Roed C, Dahl B, Obel N. Long-term prognosis and causes of death after spondylodiscitis: A Danish nationwide cohort study. Infect Dis. 2016;48(3):201-8. [Link] [DOI:10.3109/23744235.2015.1103897]
2. Alton TB, Patel AR, Bransford RJ, Bellabarba C, Lee MJ, Chapman JR. Is there a difference in neurologic outcome in medical versus early operative management of cervical epidural abscesses?. Spine J. 2015;15(1):10-7. [Link] [DOI:10.1016/j.spinee.2014.06.010]
3. Dubory A, Giorgi H, Walter A, Bouyer B, Vassal M, Zairi F, et al. Surgical-site infection in spinal injury: incidence and risk factors in a prospective cohort of 518 patients Eur Spine J. 2014;24(3):543-54. [Link] [DOI:10.1007/s00586-014-3523-4]
4. Eskesen AN, Astrup Belle M, Blomfeldt A. Predictors of one-year all-cause mortality and infection-related mortality in patients with Staphylococcus aureus bacteraemia. Infect Dis. 2018;50(10):743-8. [Link] [DOI:10.1080/23744235.2018.1470666]
5. Fei Q, Li J, Lin J, Li D, Wang B, Meng H, et al. Risk factors for surgical site infection after spinal surgery: A meta-analysis. World Neurosurg. 2016;95:507-15. [Link] [DOI:10.1016/j.wneu.2015.05.059]
6. Hikata T, Iwanami A, Hosogane N, Watanabe K, Ishii K, Nakamura M, et al. High preoperative hemoglobin A1c is a risk factor for surgical site infection after posterior thoracic and lumbar spinal instrumentation surgery. J Orthop Sci. 2014;19(2):223-8. [Link] [DOI:10.1007/s00776-013-0518-7]
7. Minakata K, Bando K, Tanaka S, Takanashi S, Konishi H, Miyamoto Y, et al. Preoperative chronic kidney disease as a strong predictor of postoperative infection and mortality after coronary artery bypass grafting. Circ J. 2014;78(9):2225-31. [Link] [DOI:10.1253/circj.CJ-14-0328]
8. Nickerson EK, Sinha R. Vertebral osteomyelitis in adults: an update. Br Med Bull. 2016;117(1):121-38. [Link] [DOI:10.1093/bmb/ldw003]
9. Puvanesarajah V, Jain A, Hess DE, Shimer AL, Shen FH, Hassanzadeh H. Complications and mortality after lumbar spinal fusion in elderly patients with late stage renal disease. Spine J. 2016;16(10):S267. [Link] [DOI:10.1016/j.spinee.2016.07.363]
10. Rutges JP, Kempen DH, van Dijk M, Oner FC. Outcome of conservative and surgical treatment of pyogenic spondylodiscitis: a systematic literature review. Eur Spine J. 2016;25:983-99. [Link] [DOI:10.1007/s00586-015-4318-y]
11. Segreto FA, Beyer GA, Grieco P, Horn SR, Bortz CA, Jalai CM, et al. Vertebral Osteomyelitis: A comparison of associated outcomes in early versus delayed surgical treatment. Int J Spine Surg. 2018;12(6):703-12. [Link] [DOI:10.14444/5088]










