GMJ Medicine
eISSN : 2626-3041
Volume 2, Issue 1 (2023)
GMJM 2023, 2(1): 9-13 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/06/29 | Accepted: 2023/01/6 | Published: 2023/02/12
Received: 2022/06/29 | Accepted: 2023/01/6 | Published: 2023/02/12
How to cite this article
Noei Alamdary S, Ghasembaglou S. Comparison of Olfactory Quality in Patients with Sinus and Nasal Polyposis Before and After Polypectomy. GMJM 2023; 2 (1) :9-13
URL: http://gmedicine.de/article-2-196-en.html
URL: http://gmedicine.de/article-2-196-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
Sh. Noei Alamdary1, Sh. Ghasembaglou *1
1- Department of Otorhinolaryngology, School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Keywords:
| Abstract (HTML) (1831 Views)
Full-Text: (714 Views)
Introduction
The sense of smell plays an important role in human life and the perception of different odors improves the quality of life. The olfactory receptors are located in the upper part of the olfactory cleft of the nose [1]. To properly understand odor, an appropriate amount of the molecules of the substance must reach the receptors and stimulate them, and then messages are sent to the brain through the olfactory nerve. Olfactory disorders come in many forms, including a decrease in sense of smell, complete loss of smell (anosmia), parosemia (change in the actual sense of smell), and phantosemia (a bad smell that does not exist). The patient's symptoms may be intermittent or permanent [2, 3].
There are a variety of causes associated with olfactory disorders. Known causes of olfactory disorders include diseases of the nose and sinuses such as sinusitis and polyps, colds (may be permanent or temporary [4], head trauma with or without a skull fracture, aging, congenital causes, exposure to toxins, nasal and brain tumors, Seizures, disorders and diseases of the nervous system such as Alzheimer's disease and Parkinson's disease, drugs and various types of nose and sinus surgeries such as rhinoplasty [5, 6].
For diagnosis after the initial examination, if necessary, olfactory tests, nasal endoscopy, CT scan or MRI are requested for the patient. The treatment of these patients depends on the underlying cause [7]. Most patients with nasal and sinus involvement will recover completely or partially by controlling inflammation or infection. In patients with severe mucosal or olfactory nerve damage, in many cases the outcome of treatment is not favorable [8].
One of the most common causes of olfactory dysfunction is nasal polyps. Nasal polyps are a very common complication in patients with symptoms of the nose, upper and lower respiratory tract, or lungs. A polyp is defined as a soft mass caused by proliferation of the lamina properia of the nasopharyngeal mucosa, and the proliferation of polyps gradually fills the mucosa of the nasal cavity or sinus [9]. As the problem worsens, the mucus appears as lumps that are similar to grape seeds and come in different colors, red, brown, pink, or gray, which is actually a polyp [10]. Various causes can cause severe swelling and polyps. Chronic infection, sensitivity to various known and unknown environmental factors, immunodeficiency, fungal infections, the presence of a foreign body and any factor that causes long-term irritation of the mucosa, can cause polyps. In some cases, no cause is found for polyps [11].
Small polyps may not cause any symptoms, but as the polyp enlarges, the patient develops symptoms. Symptoms include shortness of breath, nasal congestion, and occasional snoring, sore throat or runny nose, bad breath, dry mouth, pain or pressure in the face and nose [12]. Sometimes the polyp comes out of the nostril and creates an unpleasant appearance. In cases where the polyp is located in the back of the nose, it may hang inside the mouth and behind the palate. Severe polyps, especially in adulthood, cause changes in the appearance of the nose and face. Nasal polyps cause problems in the patient's function, especially in concentration, due to respiratory problems. It also causes limitations in exercise and strenuous activity. Treatment of polyps improves the quality of life. Of course, not all symptoms may be present in the patient [13].
There are various treatments for this disease, the most important of which is diagnosis and elimination of the underlying cause and drug treatment. Some polyps do not respond to drug treatment or recur after recovery and therefore require surgery. These include large polyps, polyps that enter the mouth from the back of the nose, and polyps that are caused by a fungal infection. Surgical treatment is performed through the nose and sinus endoscopy [14]. In this method, without making an incision in the face or inside the mouth, the polyps are removed and at the same time, the sinus opening is opened to prevent recurrence. Sometimes, to prevent recurrence, topical treatment by washing and spraying may be continued for several months after surgery [15].
Since nasal polyps have a possible role in causing olfactory disorders and olfactory disorders have an effective role in reducing the quality of life, we decided to investigate the role of surgery in the treatment of polyps and then compare the changes in the sense of smell. Therefore, the main purpose of this article is Evaluation of olfactory quality in patients with sinus and nasal polyposis before and after surgery.
Materials and Methods
Study design
This study is a descriptive-analytical study with the participation of 72 patients referred to Emma Reza Hospital (Tabriz University of Medical Sciences) during the years 2018-2020 by available and consecutive sampling method and observing the inclusion criteria / Logout done.
Inclusion/Exclusion Criteria
Inclusion criteria included patients who were candidates for polypectomy and sinus surgery, sufficient alertness to understand the technique described and consent to participate in the study; Exclusion criteria included a history of preoperative head trauma, nasal cancer, a history of five or more polypectomy procedures, and no referral for olfactory tests.
The checklist used in this study was completed in the field and interviews with patients. This questionnaire is designed based on objectives and includes demographic information (file number, age, gender, education), previous history of disease (including previous history of polyps, asthma, diabetes, hypertension, allergic rhinitis, aspirin allergy), history of drug use and It is a type of polyp (unilateral or bilateral). Also, two sections related to olfactory test before and after the operation were considered at the end of the checklist. Evaluation of olfactory quality was performed before surgery and four weeks after surgery. Odor assessment was performed by a semi-structured questionnaire on olfactory quality, taste and appetite along with a rapid olfactory diagnosis test through a researcher-patient interview. This is a standard tool for checking the level of smell and taste that is routinely used in the clinic. Based on the results of patients' olfactory diagnosis test in two ways:
1) Existence of olfactory disorder: Patients with normal olfactory versus patients with abnormal olfactory;
2) Existence of sense of smell: Patients with sense of smell are classified as patients without sense of smell.
Rapid olfactory test was performed by the kits of Saba Tajhiz Sabalan Medical Engineering Company. Each kit consists of six brown strips with different aromatic substances. One to six patients are evaluated from a bar, respectively. The test method is that after announcing the patient's readiness, a few lines were created on the brown tape with a pencil and the tape was immediately placed in front of the patient's nose. The patient was then asked to select an option from the four available options that matched the sense of smell (if the patient was unable to read the options, the options were read aloud and sequenced). It is classified as anosmia if the patient does not correctly detect any of the odors. It was classified as a normal odor if it correctly identified five of the odors. If it is among these cases, it was classified as hyposmia.
Data analysis
Data were entered into SPSS 20 software after collection. entered. Analytical analysis (McNemar test and Wilcoxon test) was used to present the results of descriptive analysis (frequency, percentage, mean, standard deviation). P Value was considered significant for less than 0.05.
Ethical considerations
After the approval of this study in the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1397.294), the objectives of the study were explained to the participants in the study and their consent was obtained.
Findings
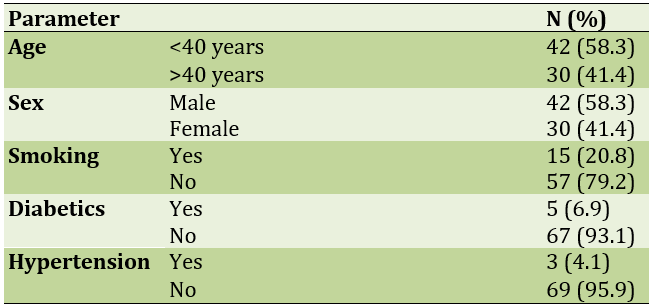
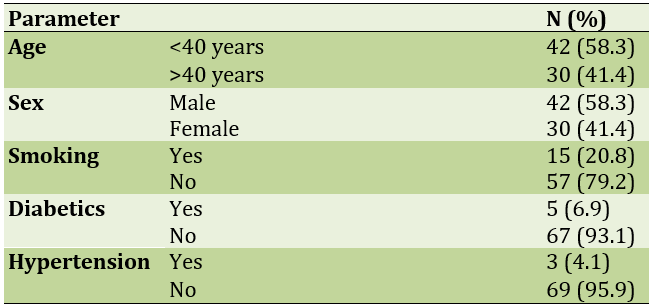
During the study period, 80 patients met the inclusion criteria and the olfactory test was performed for them. During the follow-up period, 8 patients were excluded from the study due to non-referral for the second olfactory test. Therefore, 72 patients were enrolled in the study. All patients underwent polypectomy. The mean age of patients undergoing surgery was 32.49±3.69 years. As shown in Table 1, the majority of patients were less than 40 years old and male, and the number of patients was diabetic (n=5) and hypertensive (n=3).
Table 1) Demographic information of study participants
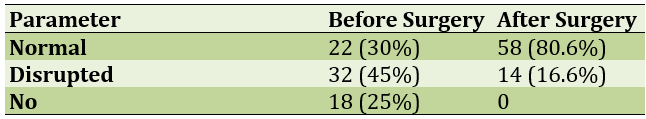
There was a history of nasal polyps in 20 participants and a history of nasal surgery in 12 people; Nasal polyps in the studied patients were bilateral in 58.3% of patients and unilateral in the rest. Comparison of the frequency of pre- and postoperative olfactory dysfunction showed that there was a significant difference between the frequency of pre- and postoperative olfactory dysfunction and postoperative olfactory quality showed a significant improvement (p<0.001 in all cases; Table 2).
Table 2) Comparison of the frequency of olfactory disorders before and after surgery
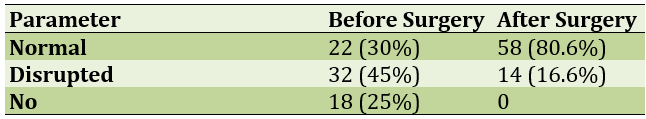
Comparison of the frequency of olfactory sense before and after surgery showed that the sense of smell was present in 75% of patients and after surgery in 100% of patients and the observed difference was significant (p=0.004).
Discussion
The aim of this study was to evaluate the olfactory quality in patients with sinus and nasal polyposis before and after endoscopic surgery. Overall, the results of this study showed that most of the patients with nasal polyps have impaired olfactory quality and in many cases there is no sense of smell in these patients. The results of this study also showed that after endoscopy, there was a sense of smell in all patients and its quality was significantly improved. In this study, the results showed that olfactory dysfunction in patients with nasal polyps has a considerable frequency [16].
In line with the results of this study, in a similar study, it was shown that olfactory function in patients with nasal polyps was compared with those without nasal obstruction. The results showed that olfactory diagnosis was better in controls than in patients. Is a nasal polyp. In fact, the obstructive effects of polyps cause olfactory disorders in patients [17].
Regarding the positive effect of endoscopic polypectomy on olfactory function, studies have been performed in the past, which in most cases have been consistent with the results of this study. A study on the effect of functional endoscopic sinus surgery on olfactory function and asthma symptoms performed on 82 patients showed that functional endoscopic sinus surgery is an effective method in the treatment of nasal polyps that is accompanied by a significant improvement in symptoms, especially the improvement of olfactory quality [18-20].
Another study on postoperative olfactory function was performed on 775 patients. The results of this study showed that olfactory function improved after rhinoplasty or sinus surgery in most cases, with the greatest improvement observed after polypectomy. Another study on olfactory function in patients with nasal polyps after endoscopic sinus surgery performed on 199 patients showed that performing endoscopic polyp surgery without the use of medical treatments improves olfactory function and sense of taste. There are two pathways to stimulate the olfactory epithelium orthonasally and retronasally. The main sense of smell and of course the sense of taste is related to the stimulation of the olfactory epithelium through the nose and therefore olfactory sense disorder is closely related to taste sensory disorder [21, 22].
There are several general theories about the cause of olfactory disorders in patients with polyps. The first theory states that the cause of olfactory dysfunction in these patients is due to the disturbance of nasal airflow, which leads to the lack of aromatic molecules (to stimulate) to the olfactory mucosa. With a decrease in airflow, histological changes include marked heterogeneity and the formation of degeneration zones. Therefore, after surgery and resection of the polyp, the airway opens and the ability to perceive smell is restored, although its quality may not be as normal as normal people [23-25].
However, the small sample size and the lack of use of the control group limit the scalability of the results. Therefore, the researchers suggest that future studies be conducted on a larger scale with the control group.
Conclusion
Overall, the results of this study show a significant improvement in the sense of smell of patients undergoing polypectomy.
Acknowledgements: None declared by the authors.
Ethical Permission: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
The sense of smell plays an important role in human life and the perception of different odors improves the quality of life. The olfactory receptors are located in the upper part of the olfactory cleft of the nose [1]. To properly understand odor, an appropriate amount of the molecules of the substance must reach the receptors and stimulate them, and then messages are sent to the brain through the olfactory nerve. Olfactory disorders come in many forms, including a decrease in sense of smell, complete loss of smell (anosmia), parosemia (change in the actual sense of smell), and phantosemia (a bad smell that does not exist). The patient's symptoms may be intermittent or permanent [2, 3].
There are a variety of causes associated with olfactory disorders. Known causes of olfactory disorders include diseases of the nose and sinuses such as sinusitis and polyps, colds (may be permanent or temporary [4], head trauma with or without a skull fracture, aging, congenital causes, exposure to toxins, nasal and brain tumors, Seizures, disorders and diseases of the nervous system such as Alzheimer's disease and Parkinson's disease, drugs and various types of nose and sinus surgeries such as rhinoplasty [5, 6].
For diagnosis after the initial examination, if necessary, olfactory tests, nasal endoscopy, CT scan or MRI are requested for the patient. The treatment of these patients depends on the underlying cause [7]. Most patients with nasal and sinus involvement will recover completely or partially by controlling inflammation or infection. In patients with severe mucosal or olfactory nerve damage, in many cases the outcome of treatment is not favorable [8].
One of the most common causes of olfactory dysfunction is nasal polyps. Nasal polyps are a very common complication in patients with symptoms of the nose, upper and lower respiratory tract, or lungs. A polyp is defined as a soft mass caused by proliferation of the lamina properia of the nasopharyngeal mucosa, and the proliferation of polyps gradually fills the mucosa of the nasal cavity or sinus [9]. As the problem worsens, the mucus appears as lumps that are similar to grape seeds and come in different colors, red, brown, pink, or gray, which is actually a polyp [10]. Various causes can cause severe swelling and polyps. Chronic infection, sensitivity to various known and unknown environmental factors, immunodeficiency, fungal infections, the presence of a foreign body and any factor that causes long-term irritation of the mucosa, can cause polyps. In some cases, no cause is found for polyps [11].
Small polyps may not cause any symptoms, but as the polyp enlarges, the patient develops symptoms. Symptoms include shortness of breath, nasal congestion, and occasional snoring, sore throat or runny nose, bad breath, dry mouth, pain or pressure in the face and nose [12]. Sometimes the polyp comes out of the nostril and creates an unpleasant appearance. In cases where the polyp is located in the back of the nose, it may hang inside the mouth and behind the palate. Severe polyps, especially in adulthood, cause changes in the appearance of the nose and face. Nasal polyps cause problems in the patient's function, especially in concentration, due to respiratory problems. It also causes limitations in exercise and strenuous activity. Treatment of polyps improves the quality of life. Of course, not all symptoms may be present in the patient [13].
There are various treatments for this disease, the most important of which is diagnosis and elimination of the underlying cause and drug treatment. Some polyps do not respond to drug treatment or recur after recovery and therefore require surgery. These include large polyps, polyps that enter the mouth from the back of the nose, and polyps that are caused by a fungal infection. Surgical treatment is performed through the nose and sinus endoscopy [14]. In this method, without making an incision in the face or inside the mouth, the polyps are removed and at the same time, the sinus opening is opened to prevent recurrence. Sometimes, to prevent recurrence, topical treatment by washing and spraying may be continued for several months after surgery [15].
Since nasal polyps have a possible role in causing olfactory disorders and olfactory disorders have an effective role in reducing the quality of life, we decided to investigate the role of surgery in the treatment of polyps and then compare the changes in the sense of smell. Therefore, the main purpose of this article is Evaluation of olfactory quality in patients with sinus and nasal polyposis before and after surgery.
Materials and Methods
Study design
This study is a descriptive-analytical study with the participation of 72 patients referred to Emma Reza Hospital (Tabriz University of Medical Sciences) during the years 2018-2020 by available and consecutive sampling method and observing the inclusion criteria / Logout done.
Inclusion/Exclusion Criteria
Inclusion criteria included patients who were candidates for polypectomy and sinus surgery, sufficient alertness to understand the technique described and consent to participate in the study; Exclusion criteria included a history of preoperative head trauma, nasal cancer, a history of five or more polypectomy procedures, and no referral for olfactory tests.
The checklist used in this study was completed in the field and interviews with patients. This questionnaire is designed based on objectives and includes demographic information (file number, age, gender, education), previous history of disease (including previous history of polyps, asthma, diabetes, hypertension, allergic rhinitis, aspirin allergy), history of drug use and It is a type of polyp (unilateral or bilateral). Also, two sections related to olfactory test before and after the operation were considered at the end of the checklist. Evaluation of olfactory quality was performed before surgery and four weeks after surgery. Odor assessment was performed by a semi-structured questionnaire on olfactory quality, taste and appetite along with a rapid olfactory diagnosis test through a researcher-patient interview. This is a standard tool for checking the level of smell and taste that is routinely used in the clinic. Based on the results of patients' olfactory diagnosis test in two ways:
1) Existence of olfactory disorder: Patients with normal olfactory versus patients with abnormal olfactory;
2) Existence of sense of smell: Patients with sense of smell are classified as patients without sense of smell.
Rapid olfactory test was performed by the kits of Saba Tajhiz Sabalan Medical Engineering Company. Each kit consists of six brown strips with different aromatic substances. One to six patients are evaluated from a bar, respectively. The test method is that after announcing the patient's readiness, a few lines were created on the brown tape with a pencil and the tape was immediately placed in front of the patient's nose. The patient was then asked to select an option from the four available options that matched the sense of smell (if the patient was unable to read the options, the options were read aloud and sequenced). It is classified as anosmia if the patient does not correctly detect any of the odors. It was classified as a normal odor if it correctly identified five of the odors. If it is among these cases, it was classified as hyposmia.
Data analysis
Data were entered into SPSS 20 software after collection. entered. Analytical analysis (McNemar test and Wilcoxon test) was used to present the results of descriptive analysis (frequency, percentage, mean, standard deviation). P Value was considered significant for less than 0.05.
Ethical considerations
After the approval of this study in the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1397.294), the objectives of the study were explained to the participants in the study and their consent was obtained.
Findings
During the study period, 80 patients met the inclusion criteria and the olfactory test was performed for them. During the follow-up period, 8 patients were excluded from the study due to non-referral for the second olfactory test. Therefore, 72 patients were enrolled in the study. All patients underwent polypectomy. The mean age of patients undergoing surgery was 32.49±3.69 years. As shown in Table 1, the majority of patients were less than 40 years old and male, and the number of patients was diabetic (n=5) and hypertensive (n=3).
Table 1) Demographic information of study participants
There was a history of nasal polyps in 20 participants and a history of nasal surgery in 12 people; Nasal polyps in the studied patients were bilateral in 58.3% of patients and unilateral in the rest. Comparison of the frequency of pre- and postoperative olfactory dysfunction showed that there was a significant difference between the frequency of pre- and postoperative olfactory dysfunction and postoperative olfactory quality showed a significant improvement (p<0.001 in all cases; Table 2).
Table 2) Comparison of the frequency of olfactory disorders before and after surgery
Comparison of the frequency of olfactory sense before and after surgery showed that the sense of smell was present in 75% of patients and after surgery in 100% of patients and the observed difference was significant (p=0.004).
Discussion
The aim of this study was to evaluate the olfactory quality in patients with sinus and nasal polyposis before and after endoscopic surgery. Overall, the results of this study showed that most of the patients with nasal polyps have impaired olfactory quality and in many cases there is no sense of smell in these patients. The results of this study also showed that after endoscopy, there was a sense of smell in all patients and its quality was significantly improved. In this study, the results showed that olfactory dysfunction in patients with nasal polyps has a considerable frequency [16].
In line with the results of this study, in a similar study, it was shown that olfactory function in patients with nasal polyps was compared with those without nasal obstruction. The results showed that olfactory diagnosis was better in controls than in patients. Is a nasal polyp. In fact, the obstructive effects of polyps cause olfactory disorders in patients [17].
Regarding the positive effect of endoscopic polypectomy on olfactory function, studies have been performed in the past, which in most cases have been consistent with the results of this study. A study on the effect of functional endoscopic sinus surgery on olfactory function and asthma symptoms performed on 82 patients showed that functional endoscopic sinus surgery is an effective method in the treatment of nasal polyps that is accompanied by a significant improvement in symptoms, especially the improvement of olfactory quality [18-20].
Another study on postoperative olfactory function was performed on 775 patients. The results of this study showed that olfactory function improved after rhinoplasty or sinus surgery in most cases, with the greatest improvement observed after polypectomy. Another study on olfactory function in patients with nasal polyps after endoscopic sinus surgery performed on 199 patients showed that performing endoscopic polyp surgery without the use of medical treatments improves olfactory function and sense of taste. There are two pathways to stimulate the olfactory epithelium orthonasally and retronasally. The main sense of smell and of course the sense of taste is related to the stimulation of the olfactory epithelium through the nose and therefore olfactory sense disorder is closely related to taste sensory disorder [21, 22].
There are several general theories about the cause of olfactory disorders in patients with polyps. The first theory states that the cause of olfactory dysfunction in these patients is due to the disturbance of nasal airflow, which leads to the lack of aromatic molecules (to stimulate) to the olfactory mucosa. With a decrease in airflow, histological changes include marked heterogeneity and the formation of degeneration zones. Therefore, after surgery and resection of the polyp, the airway opens and the ability to perceive smell is restored, although its quality may not be as normal as normal people [23-25].
However, the small sample size and the lack of use of the control group limit the scalability of the results. Therefore, the researchers suggest that future studies be conducted on a larger scale with the control group.
Conclusion
Overall, the results of this study show a significant improvement in the sense of smell of patients undergoing polypectomy.
Acknowledgements: None declared by the authors.
Ethical Permission: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
References
1. Rudmik L, Smith KA, Kilty S. Endoscopic polypectomy in the clinic: a pilot cost-effectiveness analysis. Clin Otolaryngol. 2016;41(2):110-7. [Link] [DOI:10.1111/coa.12473]
2. Velez F, Sacks H, Messina J, Malone D, Smith N, Mahmoud R. cost-effectiveness of eds-flu in sinus surgery candidates who have chronic rhinosinusitis with nasal polyps. Ann Allergy Asthma Immunol. 2018;121(5):S20-1. [Link] [DOI:10.1016/j.anai.2018.09.062]
3. Scangas GA, Lehmann AE, Remenschneider AK, Su BM, Shrime MG, Metson R. The value of frontal sinusotomy for chronic rhinosinusitis with nasal polyps-A cost utility analysis. Laryngoscope. 2018;128(1):43-51. [Link] [DOI:10.1002/lary.26783]
4. Scangas A, Remenschneider AK, Su BM, Shrime MG, Metson R. The impact of asthma on the cost effectiveness of surgery for chronic rhinosinusitis with nasal polyps. Int Forum Allergy Rhinol. 2017;7(11):1035-44. [Link] [DOI:10.1002/alr.22013]
5. Scangas GA, Remenschneider AK, Su BM, Shrime MG, Metson R. Cost utility analysis of endoscopic sinus surgery for chronic rhinosinusitis with and without nasal polyposis. Laryngoscope. 2017;127(1):29-37. [Link] [DOI:10.1002/lary.26169]
6. Rudmik L, Soler ZM, Smith TL, Mace JC, Schlosser RJ, DeConde AS. Effect of continued medical therapy on productivity costs for refractory chronic rhinosinusitis. JAMA. 2015;141(11):969-73. [Link] [DOI:10.1001/jamaoto.2015.2321]
7. Chowdhury NI, Mace JC, Smith TL, Rudmik L. What drives productivity loss in chronic rhinosinusitis? A SNOT-22 subdomain analysis. Laryngoscope. 2018:128(1):23-30. [Link] [DOI:10.1002/lary.26723]
8. Velez FF, Sacks HJ, Dennison JC, Smith N, Malone DC, Mahmoud RA. Lifetime work productivity gains among patients with chronic rhinosinusitis with nasal polyps (CRSwNP) treated with EDS-FLU. J Allergy Clin Immunol. 2019;143:AB281. [Link] [DOI:10.1016/j.jaci.2018.12.858]
9. Velez F, Sacks H, Messina J. Impact of exhalation delivery system with fluticasone on work productivity in the U.S.: results from 2 phase III trials, NAVIGATE 1 and 2. J Manag Care Spec Pharm. 2018;24:S73. [Link]
10. Philpott C, Hopkins C, Erskine S, Kumar N, Robertson A, Farboud A, et al. The burden of revision sinonasal surgery in the uk-data from the chronic rhinosinusitis epidemiology study (CRES): A cross-sectional study. BMJ. 2015;5(4):e006680. [Link] [DOI:10.1136/bmjopen-2014-006680]
11. Stein NR, Jafari A, DeConde AS. Revision rates and time to revision following endoscopic sinus surgery: A large database analysis. Laryngoscope. 2018;128(1):31-6. [Link] [DOI:10.1002/lary.26741]
12. Ference EH, Suh JD, Tan BK, Smith SS. How Often is Sinus Surgery Performed for Chronic Rhinosinusitis with versus without Nasal Polyps?. Am J Rhinol Allergy. 2018;32(1):34-9. [Link] [DOI:10.2500/ajra.2018.32.4495]
13. Mahmoud R, Palmer J, Biletch R. Healthcare for chronic rhinosinusitis (CRS) symptoms -a cross-sectional population-based survey of U.S. adults meeting symptom criteria for CRS. J Allergy Clin Immunol. 2017;139:AB68. [Link] [DOI:10.1016/j.jaci.2016.12.269]
14. Hunter TD, DeConde AS, Manes RP. Disease-related expenditures and revision rates in chronic rhinosinusitis patients after endoscopic sinus surgery. J Med Econ. 2018;21(6):610-5. [Link] [DOI:10.1080/13696998.2018.1452748]
15. Wu XF, Kong WF, Wang WH, Yuan LX, Xu HQ, Qi M, et al. Enhanced recovery after surgery protocols in functional endoscopic sinus surgery for patients with chronic rhinosinusitis with nasal polyps: a randomized clinical trial. Chin. Med. J. 2019;132:253-8. [Link] [DOI:10.1097/CM9.0000000000000060]
16. Bhattacharyya N, Villeneuve S, Joish VN, Amand C, Mannent L, Amin N, et al. Cost burden and resource utilization in patients with chronic rhinosinusitis and nasal polyps. Laryngoscope. 2019;129(9):1969-75. [Link] [DOI:10.1002/lary.27852]
17. McClure NS, Sayah FA, Xie F, Luo N, Johnson JA. Instrument-Defined Estimates of the Minimally Important Difference for EQ-5D-5L Index Scores. Value Health. 2017;20(4):644-50. [Link] [DOI:10.1016/j.jval.2016.11.015]
18. Chowdhury NI, Mace JC, Bodner TE, Alt JA, Deconde AS, et al. Investigating the minimal clinically important difference for SNOT-22 symptom domains in surgically managed chronic rhinosinusitis. Int Forum Allergy Rhinol. 2017;7(12):1149-55. [Link] [DOI:10.1002/alr.22028]
19. Toma S, Hopkins C. Stratification of SNOT-22 scores into mild, moderate or severe and relationship with other subjective instruments. Rhinology. 2016;54(2):129-33. [Link] [DOI:10.4193/Rhino15.072]
20. Erskine S, Hopkins C, Kumar N, Wilson J, Clark A, Robertson A, et al. A cross sectional analysis of a case-control study about quality of life in CRS in the UK; a comparison between CRS subtypes. Rhinology. 2016;54:311-5. [Link] [DOI:10.4193/Rhino15.361]
21. Cooper T, Greig SR, Zhang H, Seemann R, Wright ED, Vliagoftis H, et al. Objective and subjective sinonasal and pulmonary outcomes in aspirin desensitization therapy: A prospective cohort study. Auris Nasus Larynx. 2019;46(4):526-32. [Link] [DOI:10.1016/j.anl.2018.12.002]
22. Gray ST, Phillips KM, Hoehle LP, Feng AL, Yamasaki A, Caradonna DS, et al. Utilization patterns of systemic corticosteroid use for chronic rhinosinusitis. Acta Otolaryngol. 2018;138(2):153-8. [Link] [DOI:10.1080/00016489.2017.1380313]
23. Mady LJ, Schwarzbach HL, Boudreau RM, Willson TJ, Lee SE, Moore JA, et al. Air pollutants may be environmental risk factors in chronic rhinosinusitis disease progression. Int Forum Allergy Rhinol. 2018;8(3):377-84. [Link] [DOI:10.1002/alr.22052]
24. Schlosser RJ, Mulligan JK, Hyer JM, Karnezis TT, Gudis DA, Soler ZM. Air pollutants may be environmental risk factors in chronic rhinosinusitis disease progression. JAMA. 2016;142(3):731-7. [Link] [DOI:10.1001/jamaoto.2016.0927]
25. Kohli P, Schlosser RJ, Storck K, Soler ZM. Olfactory cleft computed tomography analysis and olfaction in chronic rhinosinusitis. Am J Rhinol Allergy. 2016;30(6):402-6. [Link] [DOI:10.2500/ajra.2016.30.4365]