GMJ Medicine
eISSN : 2626-3041
Volume 2, Issue 1 (2023)
GMJM 2023, 2(1): 19-22 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/08/15 | Accepted: 2023/02/6 | Published: 2023/03/29
Received: 2022/08/15 | Accepted: 2023/02/6 | Published: 2023/03/29
How to cite this article
L. S. Levels of Serum Calcium and Vitamin D in Children with Type 2 Diabetes. GMJM 2023; 2 (1) :19-22
URL: http://gmedicine.de/article-2-198-en.html
URL: http://gmedicine.de/article-2-198-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
Saboktakin L. *
Department of Otorhinolaryngology, Tabriz University Of medical Sciences, Tabriz, Iran
Keywords:
| Abstract (HTML) (1766 Views)
Full-Text: (447 Views)
Introduction
Vitamin D is one of the fat-soluble vitamins that plays an important role in the body, which involves maintaining the health of bone, teeth and joints and helping the function of the immune system. This vitamin is found in certain foods, but in the body, in the event of exposure to the sun [1].
Symptoms of vitamin D deficiency are bone pain and muscle weakness to reduce and weak immune system [2]. While prolonged shortages can cause abdominal obesity, increased blood pressure, psoriasis, osteoporosis, chronic fatigue, Alzheimer's disease, cancer and type of type 2. Vitamin D helps improve insulin sensitivity - a hormone responsible for adjusting blood glucose levels - and thus reduces the risk of insulin sensitivity, which is often a background for type 2 diabetes [3, 4].
Some researchers believe that this vitamin may help the production of insulin in the pancreas. In the ideal state of vitamin D levels should be between 20 and 56ng/ml, each of which is less than this rate as vitamin D deficiency. It is also taken. It is now clear that increasing vitamin D in the body of 60 to 80ng/ml contributes to blood glucose control, which is essential for people with diabetes [5, 6].
At the same time, with the effect of effective vitamin D receptors on insulin secretion, vitamin D also stimulates the receptors affecting insulin sensitivity [7]. Due to a complex physiological process, interference and binding between these receptors increases the number of insulin receptors in the body [8]. It gives such vitamin D to insulin sensitivity by activating the receptors to regulate the metabolism of fatty acids in the muscles and body fat. According to the relationship between vitamin D and calcium and insulin secretion, the presence of calcium for the muscles. And the fat reaction to insulin is essential that causes insulin and glucose and without vitamin D, there will be no calcium [9, 10].
Study results showed that people who receive high levels of vitamin D decreased by 43% diabetes mellitus, as well as another study showed that higher levels of vitamin D in mice were associated with a decrease in the prevalence of type 2 diabetes [11].
Due to the fact that vitamin D and calcium in diabetes can play a major role in diabetes, and informed of preventive measures, the present study aims to serum calcium and vitamin D Status in Patients with Type 2 Diabetes was done.
Instrument and Methods
Study design
This descriptive study was conducted during 2018 with participation of 122 children with type 2 diabetes. Sampling by non-probable and ready-made method was conducted by examining the records of patients with diabetes referring to the office of the physicians of the children of Tabriz University of Medical Science.
Entry and exit criteria
The criteria for entering the study included: children in two to 8 years, referring to the expertise of endocrine expertise, satisfaction with participation in the study. Exit criteria included: consumption of supplements containing calcium and vitamin D, history of liver and kidney disease, history of reacting, history of dialysis and the history of malignant cancers.
Clinical, anthropometric and biochemical evaluation
Age, sex, duration of diabetes, other diseases (based on the information contained in the case) and the anthropometric characteristics of individuals including height, weight and body mass index by nutrition, review, and in The information form was recorded. To evaluate biochemical indices (vitamin D and calcium), 100cc blood from patients in fasting state was taken by the expert in the laboratory. Blood samples were transferred to the laboratory in less than an hour at a temperature of 2 to 8°C and immediately centrifuge in the laboratory. Serum was detached until the checkout at a negative temperature of 8°C was kept.
Ethical Considerations
This study was conducted after approval in the Ethics Committee of Tabriz University of Medical Sciences (ir.tbzmed.rec.1397.870). For vitamin d and calcium tests, no cost was received; Patient parents signed consciously informed consent after explaining the goals of the research and awareness of this study.
Statistical analysis
Data were analyzed by clinical, anthropometric and biochemical studies in SPSS 21 software. Kolmogorov-Smirnov test was performed. The mean and standard deviation and frequency of sex were calculated and Pearson correlation test was used to analyze the data.
Findings
The average age of participants in the study was 5 years. The majority of them (75) were girls and the body mass index was all participants in the overweight range. The mean serum calcium level was 9.45±0.85mg/dl and the average serum levels of vitamin D were 10.99±1.14ng/ml. Serum vitamin D levels were divided into three levels of severe deficiency, mild and natural deficiency; Also, serum calcium levels were divided into two normal and abnormal levels. Body mass index and diabetes time based on vitamin d and calcium group showed a significant difference between groups; This means that the low serum levels of vitamin D and calcium are predictors of diabetes in children (Table 1).
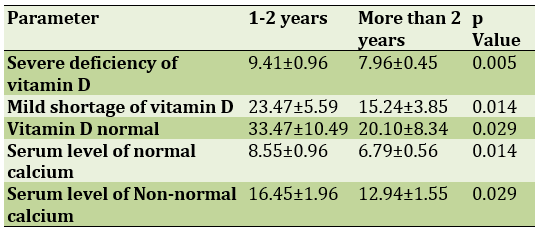
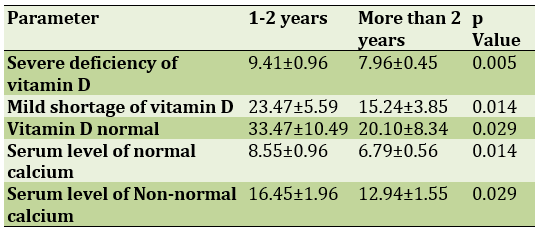
The relationship between the duration of diabetes and serum levels of vitamin d and serum calcium levels indicated that the severity of vitamin D and calcium was lower, the duration of diabetes is also higher (Table 2).
Table 1) Comparison of serum vitamin D and calcium levels based on body mass index in participants in study
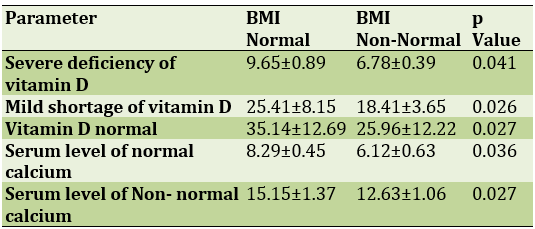
Table 2) Comparison of serum vitamin D and calcium levels based on duration of diabetes
Discussion
Many topics about calcium have been published recently. Some of this news is about calcium intake, such as the link between heart disease and calcium overdose, but it is better not to jump to conclusions and not to rule out calcium supplements [12].
Calcium is one of the most abundant minerals in the body and is responsible for the strength of bones and teeth, as well as in functions such as hormone transfer, nerve conduction and muscle function, etc. Most of the calcium in our body is stored in our bones and teeth. As we age, bone formation slows and bone extraction increases (bone loss), so calcium supplements are recommended for the elderly [13].
Calcium is found in foods such as dairy products, soy products, canned fish, dried beans, and calcium-fortified foods such as orange juice or breakfast cereals. Some nutritional recommendations list the amount of calcium you need based on age and gender, as well as the amount of calcium in your diet [14].
By looking at the nutritional information of foods, one can know the amount of calcium in it. Calcium is often given as a percentage of the daily requirement (DV%) and is less in milligrams. The allowable amount of calcium for most adults and children over 4 years is 1000 mg per day. Foods that provide 20% or more of our daily calcium needs are good sources of calcium [15].
But most people, especially postmenopausal women, split a thousand milligrams of calcium into two equal meals of 500 milligrams because at this dose more calcium is absorbed by the digestive tract. Caffeine and alcohol reduce calcium absorption. Foods containing phytic acid and oxalic acid also block calcium absorption [16]. Phytic acid is found in whole grain products that contain fiber, as well as in beans and nuts. Oxalic acid is also found in plants such as spinach and sweet potatoes. Note that you should not completely eliminate these foods from your diet because the key to good health is a balanced diet [17].
Another key issue is the presence of vitamin D, which is essential for calcium absorption. Many calcium supplements also contain vitamin D. The amount of vitamin D required also varies depending on the age and area in which people live. People who live in areas with low sunlight or people with darker skin need more vitamin D [18].
The amount of calcium and vitamin D required for each person should be determined by health counselors. Remember that there are several factors involved in determining how much calcium you need. The function of your kidneys plays a major role in calcium metabolism, and chronic kidney disease can reduce or increase the amount of calcium in your body, both of which can put your health at risk [19].
The results of a study in a very large population showed that insulin secretion improved in people who took vitamin D and calcium supplements compared to those who did not, and that Hb A1c increased less in the group taking vitamin D and calcium supplements He was from a group that did not receive vitamin D. But the researchers acknowledged that these results were not seen in people who consumed only calcium, and that calcium supplementation had no effect on any of the factors [20, 21].
One of the limitations of this study was the lack of other biochemical indicators related to calcium and vitamin D levels. It seems that other studies with more samples and a comprehensive study of serum calcium and vitamin D levels, which can be done due to seasonal changes in vitamin D at different times of the year, can clarify the serum status of calcium and vitamin D Help in children with diabetes.
Conclusion
In summary, considering the high prevalence of hypovitaminosis D in children with diabetes and considering the harmful effects of this deficiency on bone, insulin secretion and insulin sensitivity, it is necessary to find a suitable solution to solve this problem. It seems that vitamin D supplementation in children with diabetes in winter, when the rate of deficiency is very high, can be a practical solution to reduce the problems caused by this deficiency.
Acknowledgements: None declared by the authors.
Ethical Permission: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
Vitamin D is one of the fat-soluble vitamins that plays an important role in the body, which involves maintaining the health of bone, teeth and joints and helping the function of the immune system. This vitamin is found in certain foods, but in the body, in the event of exposure to the sun [1].
Symptoms of vitamin D deficiency are bone pain and muscle weakness to reduce and weak immune system [2]. While prolonged shortages can cause abdominal obesity, increased blood pressure, psoriasis, osteoporosis, chronic fatigue, Alzheimer's disease, cancer and type of type 2. Vitamin D helps improve insulin sensitivity - a hormone responsible for adjusting blood glucose levels - and thus reduces the risk of insulin sensitivity, which is often a background for type 2 diabetes [3, 4].
Some researchers believe that this vitamin may help the production of insulin in the pancreas. In the ideal state of vitamin D levels should be between 20 and 56ng/ml, each of which is less than this rate as vitamin D deficiency. It is also taken. It is now clear that increasing vitamin D in the body of 60 to 80ng/ml contributes to blood glucose control, which is essential for people with diabetes [5, 6].
At the same time, with the effect of effective vitamin D receptors on insulin secretion, vitamin D also stimulates the receptors affecting insulin sensitivity [7]. Due to a complex physiological process, interference and binding between these receptors increases the number of insulin receptors in the body [8]. It gives such vitamin D to insulin sensitivity by activating the receptors to regulate the metabolism of fatty acids in the muscles and body fat. According to the relationship between vitamin D and calcium and insulin secretion, the presence of calcium for the muscles. And the fat reaction to insulin is essential that causes insulin and glucose and without vitamin D, there will be no calcium [9, 10].
Study results showed that people who receive high levels of vitamin D decreased by 43% diabetes mellitus, as well as another study showed that higher levels of vitamin D in mice were associated with a decrease in the prevalence of type 2 diabetes [11].
Due to the fact that vitamin D and calcium in diabetes can play a major role in diabetes, and informed of preventive measures, the present study aims to serum calcium and vitamin D Status in Patients with Type 2 Diabetes was done.
Instrument and Methods
Study design
This descriptive study was conducted during 2018 with participation of 122 children with type 2 diabetes. Sampling by non-probable and ready-made method was conducted by examining the records of patients with diabetes referring to the office of the physicians of the children of Tabriz University of Medical Science.
Entry and exit criteria
The criteria for entering the study included: children in two to 8 years, referring to the expertise of endocrine expertise, satisfaction with participation in the study. Exit criteria included: consumption of supplements containing calcium and vitamin D, history of liver and kidney disease, history of reacting, history of dialysis and the history of malignant cancers.
Clinical, anthropometric and biochemical evaluation
Age, sex, duration of diabetes, other diseases (based on the information contained in the case) and the anthropometric characteristics of individuals including height, weight and body mass index by nutrition, review, and in The information form was recorded. To evaluate biochemical indices (vitamin D and calcium), 100cc blood from patients in fasting state was taken by the expert in the laboratory. Blood samples were transferred to the laboratory in less than an hour at a temperature of 2 to 8°C and immediately centrifuge in the laboratory. Serum was detached until the checkout at a negative temperature of 8°C was kept.
Ethical Considerations
This study was conducted after approval in the Ethics Committee of Tabriz University of Medical Sciences (ir.tbzmed.rec.1397.870). For vitamin d and calcium tests, no cost was received; Patient parents signed consciously informed consent after explaining the goals of the research and awareness of this study.
Statistical analysis
Data were analyzed by clinical, anthropometric and biochemical studies in SPSS 21 software. Kolmogorov-Smirnov test was performed. The mean and standard deviation and frequency of sex were calculated and Pearson correlation test was used to analyze the data.
Findings
The average age of participants in the study was 5 years. The majority of them (75) were girls and the body mass index was all participants in the overweight range. The mean serum calcium level was 9.45±0.85mg/dl and the average serum levels of vitamin D were 10.99±1.14ng/ml. Serum vitamin D levels were divided into three levels of severe deficiency, mild and natural deficiency; Also, serum calcium levels were divided into two normal and abnormal levels. Body mass index and diabetes time based on vitamin d and calcium group showed a significant difference between groups; This means that the low serum levels of vitamin D and calcium are predictors of diabetes in children (Table 1).
The relationship between the duration of diabetes and serum levels of vitamin d and serum calcium levels indicated that the severity of vitamin D and calcium was lower, the duration of diabetes is also higher (Table 2).
Table 1) Comparison of serum vitamin D and calcium levels based on body mass index in participants in study
Table 2) Comparison of serum vitamin D and calcium levels based on duration of diabetes
Discussion
Many topics about calcium have been published recently. Some of this news is about calcium intake, such as the link between heart disease and calcium overdose, but it is better not to jump to conclusions and not to rule out calcium supplements [12].
Calcium is one of the most abundant minerals in the body and is responsible for the strength of bones and teeth, as well as in functions such as hormone transfer, nerve conduction and muscle function, etc. Most of the calcium in our body is stored in our bones and teeth. As we age, bone formation slows and bone extraction increases (bone loss), so calcium supplements are recommended for the elderly [13].
Calcium is found in foods such as dairy products, soy products, canned fish, dried beans, and calcium-fortified foods such as orange juice or breakfast cereals. Some nutritional recommendations list the amount of calcium you need based on age and gender, as well as the amount of calcium in your diet [14].
By looking at the nutritional information of foods, one can know the amount of calcium in it. Calcium is often given as a percentage of the daily requirement (DV%) and is less in milligrams. The allowable amount of calcium for most adults and children over 4 years is 1000 mg per day. Foods that provide 20% or more of our daily calcium needs are good sources of calcium [15].
But most people, especially postmenopausal women, split a thousand milligrams of calcium into two equal meals of 500 milligrams because at this dose more calcium is absorbed by the digestive tract. Caffeine and alcohol reduce calcium absorption. Foods containing phytic acid and oxalic acid also block calcium absorption [16]. Phytic acid is found in whole grain products that contain fiber, as well as in beans and nuts. Oxalic acid is also found in plants such as spinach and sweet potatoes. Note that you should not completely eliminate these foods from your diet because the key to good health is a balanced diet [17].
Another key issue is the presence of vitamin D, which is essential for calcium absorption. Many calcium supplements also contain vitamin D. The amount of vitamin D required also varies depending on the age and area in which people live. People who live in areas with low sunlight or people with darker skin need more vitamin D [18].
The amount of calcium and vitamin D required for each person should be determined by health counselors. Remember that there are several factors involved in determining how much calcium you need. The function of your kidneys plays a major role in calcium metabolism, and chronic kidney disease can reduce or increase the amount of calcium in your body, both of which can put your health at risk [19].
The results of a study in a very large population showed that insulin secretion improved in people who took vitamin D and calcium supplements compared to those who did not, and that Hb A1c increased less in the group taking vitamin D and calcium supplements He was from a group that did not receive vitamin D. But the researchers acknowledged that these results were not seen in people who consumed only calcium, and that calcium supplementation had no effect on any of the factors [20, 21].
One of the limitations of this study was the lack of other biochemical indicators related to calcium and vitamin D levels. It seems that other studies with more samples and a comprehensive study of serum calcium and vitamin D levels, which can be done due to seasonal changes in vitamin D at different times of the year, can clarify the serum status of calcium and vitamin D Help in children with diabetes.
Conclusion
In summary, considering the high prevalence of hypovitaminosis D in children with diabetes and considering the harmful effects of this deficiency on bone, insulin secretion and insulin sensitivity, it is necessary to find a suitable solution to solve this problem. It seems that vitamin D supplementation in children with diabetes in winter, when the rate of deficiency is very high, can be a practical solution to reduce the problems caused by this deficiency.
Acknowledgements: None declared by the authors.
Ethical Permission: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
References
1. Gupta G, de Jesus Andreoli Pinto T, Chellappan DK, Mishra A, Malipeddi H, Dua K. A clinical update on metformin and lung cancer in diabetic patients. Panminerva Med. 2018;60(2):70-5. [Link] [DOI:10.23736/S0031-0808.18.03394-3]
2. Xin GL, Khee YP, Ying TY, Chellian J, Gupta G,. Kunnath AP, et al. Current status on immunological therapies for type 1 Diabetes Mellitus. Curr Diab Rep. 2019;19(5);22. [Link] [DOI:10.1007/s11892-019-1144-3]
3. Miettinen ME, Smart MC, Kinnunen L, Harjutsalo V, Reinert-Hartwall L, Ylivinkka I, et al. Genetic determinants of serum 25-hydroxyvitamin D concentration during pregnancy and type 1 diabetes in the child. PloS One. 2017;12:e0184942. [Link] [DOI:10.1371/journal.pone.0184942]
4. Penna-Martinez M, Badenhoop K. Inherited variation in Vitamin D Genes and Type 1 Diabetes predisposition. Genes. 2017;8(4):125. [Link] [DOI:10.3390/genes8040125]
5. Nam HK, Rhie YJ, Lee YH. Vitamin D level and gene polymorphisms in Korean children with type 1 diabetes. Pediatric Diabetes, 2019;20(6):750-8. [Link] [DOI:10.1111/pedi.12878]
6. Ahmed AE, Sakhr HM, Hassan MH, El-Amir MI, Ameen HH. Vitamin D receptor rs7975232, rs731236 and rs1544410 single nucleotide polymorphisms, and 25-hydroxyvitamin D levels in Egyptian children with type 1 diabetes mellitus: effect of vitamin D co-therapy. Diabetes Metabolic Syndr Obes. 2019;12:703-16. [Link] [DOI:10.2147/DMSO.S201525]
7. Habibian N, Amoli MM, Abbasi F, Rabbani A, Alipour A, Sayarifard F, et al. Role of vitamin D and vitamin D receptor gene polymorphisms on residual beta cell function in children with type 1 diabetes mellitus. Pharmacological Rep. 2019;71:282-8. [Link] [DOI:10.1016/j.pharep.2018.12.012]
8. Rasoul MA, Haider MZ, Al-Mahdi M, Al-Kandari H, Dhaunsi GS. Relationship of four vitamin D receptor gene polymorphisms with type 1 diabetes mellitus susceptibility in Kuwaiti children. BMC Pediatrics. 2019;19:71. [Link] [DOI:10.1186/s12887-019-1448-0]
9. Ali R, Fawzy I, Mohsen I, Settin A. Evaluation of vitamin D receptor gene polymorphisms (Fok-I and Bsm-I) in T1DM Saudi children. J Clin Lab Anal. 2018;32:e22397. [Link] [DOI:10.1002/jcla.22397]
10. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ. 2015;349:g7647. [Link] [DOI:10.1136/bmj.g7647]
11. Zhang Q, Jin Y, Li X, Peng X, Peng N, Song J, et al. Plasminogen activator inhibitor-1 (PAI-1) 4G/5G promoter polymorphisms and risk of venous thromboembolism-a meta-analysis and systematic review. VASA. 2020;49(2):141-6. [Link] [DOI:10.1024/0301-1526/a000839]
12. Zhang W, Xu Y. Association between Vitamin D receptor gene polymorphism rs2228570 and allergic rhinitis. Pharmgenomics Pers Med. 2020;13:327-35. [Link] [DOI:10.2147/PGPM.S262402]
13. Al-Eisa AA, Haider MZ. Vitamin D receptor gene TaqI and Apal polymorphisms and steroid responsiveness in childhood idiopathic nephrotic syndrome. Int J Nephrol Renovasc Dis. 2016;9:187-92. [Link] [DOI:10.2147/IJNRD.S111538]
14. Rejnmark L, Bislev LS, Cashman KD, Eiríksdottir G, Gaksch M, Grübler M, et al. Non-skeletal health effects of vitamin D supplementation: A systematic review on findings from meta-analyses summarizing trial data. PLoS One. 2017;12:e0180512. [Link] [DOI:10.1371/journal.pone.0180512]
15. Cashman KD, Dowling KG, Škrabáková Z, Gonzalez-Gross M, Valtueña J, De Henauw S, et al. Vitamin D deficiency in Europe: pandemic?. Am J Clin Nutr. 2016;103:1033-44. [Link] [DOI:10.3945/ajcn.115.120873]
16. Sethuraman U, Zidan MA, Hanks L, Bagheri M, Ashraf A. Impact of vitamin D treatment on 25 hydroxy vitamin D levels and insulin homeostasis in obese African American adolescents in a randomized trial. J Clin Transl Endocrinol. 2018;12:13-9. [Link] [DOI:10.1016/j.jcte.2018.03.002]
17. Magge SN, Prasad D, Zemel BS, Kelly A. Vitamin D3 supplementation in obese, African-American, vitamin D deficient adolescents. J Clin Transl Endocrinol. 2018;12:1-7. [Link] [DOI:10.1016/j.jcte.2018.03.001]
18. Brar PC, Contreras M, Fan X, Visavachaipan N. Effect of one time high dose "stoss therapy" of vitamin D on glucose homeostasis in high risk obese adolescents. Arch Endocrinol Metab. 2018;62(2):193-200. [Link] [DOI:10.20945/2359-3997000000024]
19. Smith TJ, Tripkovic L, Hauger H, Damsgaard CT, Mølgaard C, Lanham-New SA, et al. Winter cholecalciferol supplementation at 51°n has no effect on markers of cardiometabolic risk in healthy adolescents aged 14-18 years. J Nutr. 2018;148(8):1269-75. [Link] [DOI:10.1093/jn/nxy079]
20. Hauger H, Mølgaard C, Mortensen C, Ritz C, Frøkiær H, Smith TJ, et al. Winter cholecalciferol supplementation at 55°n has no effect on markers of cardiometabolic risk in healthy children aged 4-8 years. J Nutr. 2018;148(8):1261-8. [Link] [DOI:10.1093/jn/nxy080]
21. Ferira AJ, Laing EM, Hausman DB, Hall DB, McCabe GP, Martin BR, et al. Vitamin D Supplementation Does Not Impact Insulin Resistance in Black and White Children. J Clin Endocrinol Metab. 2016;101(4):1710-8. [Link] [DOI:10.1210/jc.2015-3687]