GMJ Medicine
eISSN : 2626-3041
Volume 2, Issue 3 (2023)
GMJM 2023, 2(3): 71-75 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/12/5 | Accepted: 2023/06/26 | Published: 2023/07/29
Received: 2022/12/5 | Accepted: 2023/06/26 | Published: 2023/07/29
How to cite this article
Noei Alamdary S, Ghasembaglou S. Performance of the Eustachal Tube and the Middle Ear Pressure After Sepotoplasty Surgery. GMJM 2023; 2 (3) :71-75
URL: http://gmedicine.de/article-2-200-en.html
URL: http://gmedicine.de/article-2-200-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
Sh. Noei Alamdary1, Sh. Ghasembaglou *1
1- Department of Otorhinolaryngology, School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Keywords:
| Abstract (HTML) (1483 Views)
Full-Text: (630 Views)
Introduction
The nasal septum has many functions, including the division of the nasal airway to two distinct cavities, supporting the dosomes, and the preservation of columla and nasal tip. Septal deviation can be detected clinically or using radiological tests. In an educational study, nasal deviation in the general population was reported using 40% CT scan [1]. Septal deviation is one of the common causes of the unilateral blockage of the nasal airway, which may lead to trauma to nose and the middle part of the face. Trauma during birth, due to the use of instability, can cause septum damage, which may result in the early deviation of the septum or the late deviation that does not appear until the rapid growth stage of puberty [2, 3].
Bone and mucosal hypertrophy of the tentacle is considered a compensatory state and is seen in patients whose septum diversion is significantly large from the large tentacle. Patients who complain of nasal obstruction, and this complaint is consistent with the findings of the physical examination of the nose, often leads to sepoplasty [4]. However, some patients with severe septum deviations have no symptoms or have mild symptoms, and in contrast to some patients with brief septum deviation, complaints. Septoplasty will modify the nasal airway only when it is possible to flow the air naturally into the nose. The conservative surgery of tentacles is a contributor with septum surgery [5].
The performance of the pipe is balancing the middle ear pressure, protecting the middle ear and muscle clairness. The pipe is located on the skull base and the anterior part of the middle ear cavity is connected to nasopharynx [5]. The mouth of the pipe is located in the lateral wall of the nasopharynx behind the posterior bottom of the lower turbine. In non-negational changes, pressure, such as airplane, oxygen therapy and diving in water, is stressed under stress [6]. This sometimes causes barotruma to the middle ear, such as middle ear opiogenesis, bleeding, hemotapan, perforation of thymoman curtain and even fistula of lymph. The causes of the dysfunction of the performance of the pipe can be mechanically (intertamine or extraneous) or functional. The causes of intercolamine include polyps, mucosal inflammation, middle ear pathology. The causes of extrapoline include adenoid hypertrophy, nasopharyngeal neoplasm. Other effective factors known on the performance of the pipe of the pipeline include: Seminazal disease, allergies, cranofascial anomalies such as Down syndrome and cleft palate, extra reflux of oshegal, genetic talent and racial differences [7].
Clinical use of the performance tests of the pipe is limited today. In general, there are two types of testing of the pipe performance: tests that measure air from the tube and tests that measure the active opening of the pipe muscles. Performing a tympanometer along with these tests is a lateral measurement to determine the flow of acoustic energy from the mid-ear system and indirectly specifies the performance of the estimation of the estimator with the measurement of the middle ear pressure [8]. Tempanometric can be done alongside the performance tests of the pipe and examined the changes in the middle ear pressure. In the Valgesal test, the patient takes its nose and is working with the mouthpiece to exhale and sends air into the tube. In the Toynbee test, the patient performs swallowing with the nose. Test Toynbee opens the span of the pipe [9].
The tympanometry is performed by inserting a probe into the outer ear canal so that it completely blocks it, and the canal air pressure changes in a positive or negative direction relative to the ambient air pressure. The amount of acoustic energy reflected from the tympanic membrane is measured, which indicates information about the transmission characteristics of the middle ear. The tympanometry provides information about middle ear pressure, eustachian tube function, tympanic membrane motility and health, and bone chain health [10].
The tympanogram can be seen in tympanometry in three ways: Type A represents the normal pressure in the middle ear. Type B tympanograms may be seen in cases of otitis media with effusion, tympanic cavity space lesions, and perforation of the tympanic membrane. Type C indicates negative middle ear pressure and displacement of the tympanogram peak toward negative pressure and indicates Eustachian tube dysfunction [11, 12].
A type A tympanogram with maximum compliance at a pressure of +25 to -150mmH2O shows the normal pressure of the middle ear and indicates the normal function of the Eustachian tube. Middle ear pressure less than -150mmH2O indicates Eustachian tube dysfunction. The middle ear naturally loses gas through diffusion, and this lost gas is replaced by the Eustachian tube. When this system has a problem, the result is negative pressure in the middle ear. Pneumatic mastoid acts as a balancer to protect against this phenomenon [13].
In fact, the pressure in the middle ear is regulated by two mechanisms:
1) more with the opening of the Eustachian tube; and
2) less with the gas exchange of the mastoid mucosa.
The middle ear pressure physiologically changes during the day by changing position from standing to lying and performing various maneuvers. Many inflammatory diseases of the middle ear are attributed to Eustachian tube dysfunction, and most benign and malignant diseases of the synonasal system lead to Eustachian tube dysfunction [14].
The role of nasal septal deviation and surgical treatment on Eustachian tube function and middle ear pressure is still in question. By doing this study, the above question can be answered to some extent and if it is proven that septovlasty surgery has a significant effect on the function of the Eustachian tube and middle ear pressure, the necessity of performing the above operation before performing important ear surgeries, especially tympanoplasty, can be emphasized.
Instrument and Methods
Study design
In this prospective cohort study, 70 patients between 18 and 65 years old who referred to Imam Reza and Sina Hospital (Tabriz University of Medical Sciences) during 2018 with a complaint of unilateral or bilateral nasal congestion. They had severe nasal septal deviation on examination and underwent surgery to correct nasal septal deviation (septoplasty) and were included in the study by available sampling method. In this study, the independent variables of severe deviation of the nasal septum to the extent that it caused nasal obstruction and the dependent variables of Eustachian tube function and middle ear pressure and the underlying variables of age and sex were considered.
Inclusion/Exclusion Criteria
Inclusion criteria include patients with persistent unilateral or bilateral nasal congestion who have severe septal deviation on examination. They were over 18 years old and under 65 years old. Exclusion criteria are: any congenital or acquired disease of the nose and sinuses other than nasal septal deviation, such as patients with severe nasal septal deviation, nasal polyps or adenoid hypertrophy, or allergic rhinitis, or chronic rhinosinusitis. Patients with a history of chronic otitis media or tympanic membrane rupture. Patients with a history of rhinoplasty or ear surgery.
Procedure
Patients who complained of nasal congestion during one year referred to the ENT clinic of Imam Reza and Sina hospitals (Tabriz University of Medical Sciences) and in the examination of severe deviation of the nasal septum to the extent that obstruction of the nose and underwent septoplasty surgery were evaluated by tympanometric tests and Eustachian tube function before and after septoplasty, and the results of these tests were entered in a checklist. Patients' information including age, sex, type of septal deviation, date of surgery, date of referral after surgery, tympanometry before and after surgery, Eustachian tube function before and after surgery were recorded. In this study, to accurately determine nasal deviation using Pledget impregnated with phenylephrine, the nasal cavities of patients were shrinked and the entire nasal space on both sides was observed by anterior rhinoscopy and endoscopy. If chronic rhinosinusitis was suspected after taking a history and physical examination of patients, a CT scan of the paranasal sinuses was requested to rule out a diagnosis. In this study, middle ear pressure and Eustachian tube function were evaluated before septoplasty and three to six months after surgery. In this study, MADSEN tympanometric device model ZODIAC901 made in Denmark was used to evaluate the middle ear pressure. Middle ear pressure was measured at rest during Valsalva and Toynbee maneuvers and was displayed in DaPa (Deca Pascal). To increase the accuracy of tympanometry study of all patients was performed by an audiologist. Also, in cases where the patient had respiratory problems and nasal congestion when he referred for a postoperative tympanometric test, the tympanometric test was not performed or was postponed to another time. Due to the fact that most of the patients in the study had difficulty performing the Valsalva test and were not able to cooperate enough to perform the test correctly, the Toynbee test, which was easily performed, was considered to evaluate the performance of the Eustachian tube.
Ethical considerations
All patients completed the informed consent form and no additional costs were imposed on patients to participate in the study.
Data analysis
The collected data were entered into SPSS 20 software. Mean and standard deviation, frequency and percentage were used to display demographic information. T-test was used to compare the data. The p<0.05 considered significant.
Findings
Seventy patients were analyzed from which 14 patients had bilateral nasal obstruction. Therefore, for these patients, both sides were considered as obstruction sides, and thus there are 84 deviations of the nasal septum and 56 opposite sides of the septal deviation. The prevalence of men and women in this study was 80% and 20%, respectively, which is four times more than men. The type of septal deviation is unilateral and bilateral, 80% and 20%, respectively. The side of septal deviation is that 20% of people have bilateral deviation, 47.1% of people have right deviation and 32.9% of people have left deviation. The mean age of the subjects was 27.81±3.42 years. The mean referral time after septoplasty of 70 patients was 110.48±5.11 days.
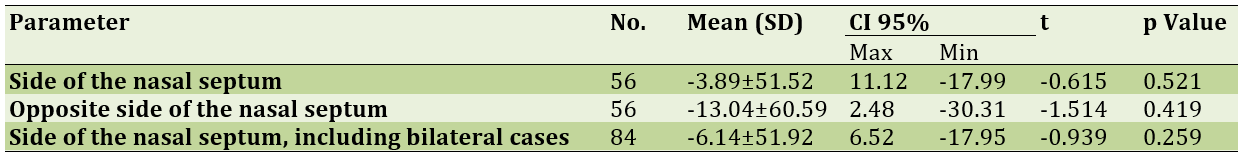
To compare the function of the Eustachian tube
before and after septoplasty on the deviant side and the opposite side of the deviation, 14 patients with bilateral obstruction were excluded from a total of 70 patients (Table 1).
Table 1) Evaluation of preliminary results of Eustachian tube function, before and after septoplasty in the deviation and opposite direction of nasal septum deviation by ETFT
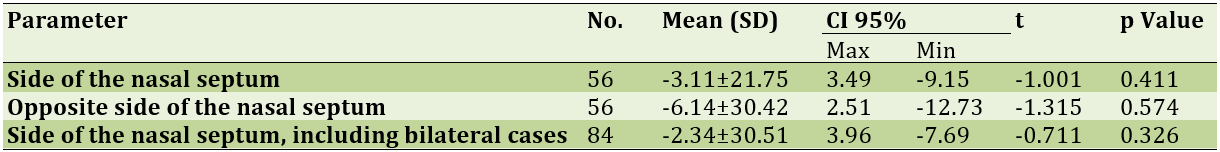
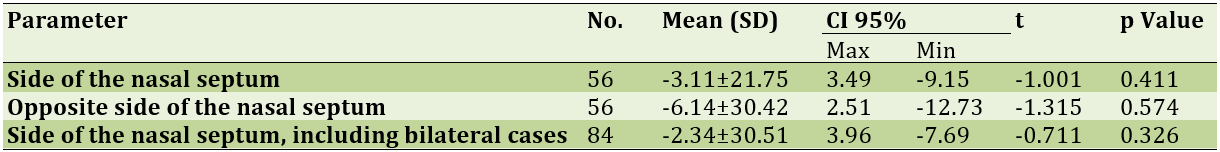
In the next analysis, 14 patients with deviation on both sides of the nasal septum were included in the study. As a result, samples containing 84 sides of the nasal septum that included deviation were also analyzed. After septoplasty by Eustachian tube function, for 56 patients on the opposite side of the nasal septum and on the opposite side of the nasal septum, 14 patients with 14 patients with bilateral deviation were removed, -3.89±51.52 and -13.04±60.59, respectively. These values for 84 patients including 14 patients with bilateral deviation were -6.14±51.92 (Table 2).
Table 2) Evaluation of preliminary results of Middle ear pressure, before and after septoplasty in the deviation and opposite direction of nasal septum deviation by ETFT
Discussion
Some researchers believe that rhinoplasty will reduce the adverse effects of nasal problems on the ear, while others believe that the malfunction of the Eustachian tube is not a barrier to middle ear surgery, especially tympanoplasty. They do not even consider it necessary to perform middle ear surgeries to evaluate the function of the Eustachian tube. In a study aimed at the effect of nasal septal deviation on middle ear pressure, it was found that there was no significant difference between the mean middle ear air pressure before and after septoplasty surgery in patients with severe and complete deviation of one side of the nose. Be consistent with the results of our study.
In a prospective study of 40 patients with septal deformity and turbinate hypertrophy, postoperative results of Eustachian tube function tests were significantly better than preoperative cases, but there was a significant difference between the mean ear pressure. The median before and after surgery was not seen to be consistent with the results of our study and in the same direction. In a study of 40 patients, it was found that the pressure in the ear on the side of the nasal obstruction increased significantly before surgery and the middle ear after surgery; The results of this study are not in line with our study [15-17].
Due to the fact that most patients had difficulty performing the Valsalva test and did not have the necessary cooperation, the Toynbee test was considered as a test to evaluate the performance of the Eustachian tube. Correction of the enlarged lower tentacle on the opposite side of the deviation was an adjunct to septal surgery to reduce obstructive symptoms. Correction of the enlarged lower tentacle on the opposite side of the deviation was not considered a standard for excluding patients [18, 19].
Based on this study, it was found that there was no significant difference between the mean air pressure of the middle ear on the deviated side of the nasal septum and on the opposite side of the deviation, before and after septoplasty surgery. Also, there was no significant difference between the function of the Eustachian tube on the deviated side of the nasal septum and on the opposite side of the deviation, before and after septoplasty surgery [20].
The number of samples is very small and also the lack of use of Valsalva test due to patients' intolerance of the limitations and weaknesses of the present study. It is suggested that in future studies, the number of patients admitted to the study be increased and these patients be followed up for a longer period of time. Also, considering that the most common complication of septoplasty is the continuation of patients' complaints of nasal obstruction and other complications such as septal perforation and changes in the shape of the nose (such as nasal ptosis and saddle formation) may occur following septoplasty surgery. Further studies of these complications should be considered.
Conclusion
Septoplasty in patients with nasal congestion due to nasal septal deviation who had no middle ear pathology did not change the middle ear pressure and Eustachian tube function after 3-6 months. Finally, based on this study and similar studies, it can be concluded that septoplasty surgery does not have a significant effect on Eustachian tube function and middle ear pressure, and septoplasty surgery is not necessary before ear surgeries such as tympanoplasty.
Acknowledgements: None declared by the authors.
Ethical Permission: This study was conducted after approval by the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.1292) and in coordination with the officials of Sina and Imam Reza hospitals.
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
The nasal septum has many functions, including the division of the nasal airway to two distinct cavities, supporting the dosomes, and the preservation of columla and nasal tip. Septal deviation can be detected clinically or using radiological tests. In an educational study, nasal deviation in the general population was reported using 40% CT scan [1]. Septal deviation is one of the common causes of the unilateral blockage of the nasal airway, which may lead to trauma to nose and the middle part of the face. Trauma during birth, due to the use of instability, can cause septum damage, which may result in the early deviation of the septum or the late deviation that does not appear until the rapid growth stage of puberty [2, 3].
Bone and mucosal hypertrophy of the tentacle is considered a compensatory state and is seen in patients whose septum diversion is significantly large from the large tentacle. Patients who complain of nasal obstruction, and this complaint is consistent with the findings of the physical examination of the nose, often leads to sepoplasty [4]. However, some patients with severe septum deviations have no symptoms or have mild symptoms, and in contrast to some patients with brief septum deviation, complaints. Septoplasty will modify the nasal airway only when it is possible to flow the air naturally into the nose. The conservative surgery of tentacles is a contributor with septum surgery [5].
The performance of the pipe is balancing the middle ear pressure, protecting the middle ear and muscle clairness. The pipe is located on the skull base and the anterior part of the middle ear cavity is connected to nasopharynx [5]. The mouth of the pipe is located in the lateral wall of the nasopharynx behind the posterior bottom of the lower turbine. In non-negational changes, pressure, such as airplane, oxygen therapy and diving in water, is stressed under stress [6]. This sometimes causes barotruma to the middle ear, such as middle ear opiogenesis, bleeding, hemotapan, perforation of thymoman curtain and even fistula of lymph. The causes of the dysfunction of the performance of the pipe can be mechanically (intertamine or extraneous) or functional. The causes of intercolamine include polyps, mucosal inflammation, middle ear pathology. The causes of extrapoline include adenoid hypertrophy, nasopharyngeal neoplasm. Other effective factors known on the performance of the pipe of the pipeline include: Seminazal disease, allergies, cranofascial anomalies such as Down syndrome and cleft palate, extra reflux of oshegal, genetic talent and racial differences [7].
Clinical use of the performance tests of the pipe is limited today. In general, there are two types of testing of the pipe performance: tests that measure air from the tube and tests that measure the active opening of the pipe muscles. Performing a tympanometer along with these tests is a lateral measurement to determine the flow of acoustic energy from the mid-ear system and indirectly specifies the performance of the estimation of the estimator with the measurement of the middle ear pressure [8]. Tempanometric can be done alongside the performance tests of the pipe and examined the changes in the middle ear pressure. In the Valgesal test, the patient takes its nose and is working with the mouthpiece to exhale and sends air into the tube. In the Toynbee test, the patient performs swallowing with the nose. Test Toynbee opens the span of the pipe [9].
The tympanometry is performed by inserting a probe into the outer ear canal so that it completely blocks it, and the canal air pressure changes in a positive or negative direction relative to the ambient air pressure. The amount of acoustic energy reflected from the tympanic membrane is measured, which indicates information about the transmission characteristics of the middle ear. The tympanometry provides information about middle ear pressure, eustachian tube function, tympanic membrane motility and health, and bone chain health [10].
The tympanogram can be seen in tympanometry in three ways: Type A represents the normal pressure in the middle ear. Type B tympanograms may be seen in cases of otitis media with effusion, tympanic cavity space lesions, and perforation of the tympanic membrane. Type C indicates negative middle ear pressure and displacement of the tympanogram peak toward negative pressure and indicates Eustachian tube dysfunction [11, 12].
A type A tympanogram with maximum compliance at a pressure of +25 to -150mmH2O shows the normal pressure of the middle ear and indicates the normal function of the Eustachian tube. Middle ear pressure less than -150mmH2O indicates Eustachian tube dysfunction. The middle ear naturally loses gas through diffusion, and this lost gas is replaced by the Eustachian tube. When this system has a problem, the result is negative pressure in the middle ear. Pneumatic mastoid acts as a balancer to protect against this phenomenon [13].
In fact, the pressure in the middle ear is regulated by two mechanisms:
1) more with the opening of the Eustachian tube; and
2) less with the gas exchange of the mastoid mucosa.
The middle ear pressure physiologically changes during the day by changing position from standing to lying and performing various maneuvers. Many inflammatory diseases of the middle ear are attributed to Eustachian tube dysfunction, and most benign and malignant diseases of the synonasal system lead to Eustachian tube dysfunction [14].
The role of nasal septal deviation and surgical treatment on Eustachian tube function and middle ear pressure is still in question. By doing this study, the above question can be answered to some extent and if it is proven that septovlasty surgery has a significant effect on the function of the Eustachian tube and middle ear pressure, the necessity of performing the above operation before performing important ear surgeries, especially tympanoplasty, can be emphasized.
Instrument and Methods
Study design
In this prospective cohort study, 70 patients between 18 and 65 years old who referred to Imam Reza and Sina Hospital (Tabriz University of Medical Sciences) during 2018 with a complaint of unilateral or bilateral nasal congestion. They had severe nasal septal deviation on examination and underwent surgery to correct nasal septal deviation (septoplasty) and were included in the study by available sampling method. In this study, the independent variables of severe deviation of the nasal septum to the extent that it caused nasal obstruction and the dependent variables of Eustachian tube function and middle ear pressure and the underlying variables of age and sex were considered.
Inclusion/Exclusion Criteria
Inclusion criteria include patients with persistent unilateral or bilateral nasal congestion who have severe septal deviation on examination. They were over 18 years old and under 65 years old. Exclusion criteria are: any congenital or acquired disease of the nose and sinuses other than nasal septal deviation, such as patients with severe nasal septal deviation, nasal polyps or adenoid hypertrophy, or allergic rhinitis, or chronic rhinosinusitis. Patients with a history of chronic otitis media or tympanic membrane rupture. Patients with a history of rhinoplasty or ear surgery.
Procedure
Patients who complained of nasal congestion during one year referred to the ENT clinic of Imam Reza and Sina hospitals (Tabriz University of Medical Sciences) and in the examination of severe deviation of the nasal septum to the extent that obstruction of the nose and underwent septoplasty surgery were evaluated by tympanometric tests and Eustachian tube function before and after septoplasty, and the results of these tests were entered in a checklist. Patients' information including age, sex, type of septal deviation, date of surgery, date of referral after surgery, tympanometry before and after surgery, Eustachian tube function before and after surgery were recorded. In this study, to accurately determine nasal deviation using Pledget impregnated with phenylephrine, the nasal cavities of patients were shrinked and the entire nasal space on both sides was observed by anterior rhinoscopy and endoscopy. If chronic rhinosinusitis was suspected after taking a history and physical examination of patients, a CT scan of the paranasal sinuses was requested to rule out a diagnosis. In this study, middle ear pressure and Eustachian tube function were evaluated before septoplasty and three to six months after surgery. In this study, MADSEN tympanometric device model ZODIAC901 made in Denmark was used to evaluate the middle ear pressure. Middle ear pressure was measured at rest during Valsalva and Toynbee maneuvers and was displayed in DaPa (Deca Pascal). To increase the accuracy of tympanometry study of all patients was performed by an audiologist. Also, in cases where the patient had respiratory problems and nasal congestion when he referred for a postoperative tympanometric test, the tympanometric test was not performed or was postponed to another time. Due to the fact that most of the patients in the study had difficulty performing the Valsalva test and were not able to cooperate enough to perform the test correctly, the Toynbee test, which was easily performed, was considered to evaluate the performance of the Eustachian tube.
Ethical considerations
All patients completed the informed consent form and no additional costs were imposed on patients to participate in the study.
Data analysis
The collected data were entered into SPSS 20 software. Mean and standard deviation, frequency and percentage were used to display demographic information. T-test was used to compare the data. The p<0.05 considered significant.
Findings
Seventy patients were analyzed from which 14 patients had bilateral nasal obstruction. Therefore, for these patients, both sides were considered as obstruction sides, and thus there are 84 deviations of the nasal septum and 56 opposite sides of the septal deviation. The prevalence of men and women in this study was 80% and 20%, respectively, which is four times more than men. The type of septal deviation is unilateral and bilateral, 80% and 20%, respectively. The side of septal deviation is that 20% of people have bilateral deviation, 47.1% of people have right deviation and 32.9% of people have left deviation. The mean age of the subjects was 27.81±3.42 years. The mean referral time after septoplasty of 70 patients was 110.48±5.11 days.
To compare the function of the Eustachian tube
before and after septoplasty on the deviant side and the opposite side of the deviation, 14 patients with bilateral obstruction were excluded from a total of 70 patients (Table 1).
Table 1) Evaluation of preliminary results of Eustachian tube function, before and after septoplasty in the deviation and opposite direction of nasal septum deviation by ETFT
In the next analysis, 14 patients with deviation on both sides of the nasal septum were included in the study. As a result, samples containing 84 sides of the nasal septum that included deviation were also analyzed. After septoplasty by Eustachian tube function, for 56 patients on the opposite side of the nasal septum and on the opposite side of the nasal septum, 14 patients with 14 patients with bilateral deviation were removed, -3.89±51.52 and -13.04±60.59, respectively. These values for 84 patients including 14 patients with bilateral deviation were -6.14±51.92 (Table 2).
Table 2) Evaluation of preliminary results of Middle ear pressure, before and after septoplasty in the deviation and opposite direction of nasal septum deviation by ETFT
Discussion
Some researchers believe that rhinoplasty will reduce the adverse effects of nasal problems on the ear, while others believe that the malfunction of the Eustachian tube is not a barrier to middle ear surgery, especially tympanoplasty. They do not even consider it necessary to perform middle ear surgeries to evaluate the function of the Eustachian tube. In a study aimed at the effect of nasal septal deviation on middle ear pressure, it was found that there was no significant difference between the mean middle ear air pressure before and after septoplasty surgery in patients with severe and complete deviation of one side of the nose. Be consistent with the results of our study.
In a prospective study of 40 patients with septal deformity and turbinate hypertrophy, postoperative results of Eustachian tube function tests were significantly better than preoperative cases, but there was a significant difference between the mean ear pressure. The median before and after surgery was not seen to be consistent with the results of our study and in the same direction. In a study of 40 patients, it was found that the pressure in the ear on the side of the nasal obstruction increased significantly before surgery and the middle ear after surgery; The results of this study are not in line with our study [15-17].
Due to the fact that most patients had difficulty performing the Valsalva test and did not have the necessary cooperation, the Toynbee test was considered as a test to evaluate the performance of the Eustachian tube. Correction of the enlarged lower tentacle on the opposite side of the deviation was an adjunct to septal surgery to reduce obstructive symptoms. Correction of the enlarged lower tentacle on the opposite side of the deviation was not considered a standard for excluding patients [18, 19].
Based on this study, it was found that there was no significant difference between the mean air pressure of the middle ear on the deviated side of the nasal septum and on the opposite side of the deviation, before and after septoplasty surgery. Also, there was no significant difference between the function of the Eustachian tube on the deviated side of the nasal septum and on the opposite side of the deviation, before and after septoplasty surgery [20].
The number of samples is very small and also the lack of use of Valsalva test due to patients' intolerance of the limitations and weaknesses of the present study. It is suggested that in future studies, the number of patients admitted to the study be increased and these patients be followed up for a longer period of time. Also, considering that the most common complication of septoplasty is the continuation of patients' complaints of nasal obstruction and other complications such as septal perforation and changes in the shape of the nose (such as nasal ptosis and saddle formation) may occur following septoplasty surgery. Further studies of these complications should be considered.
Conclusion
Septoplasty in patients with nasal congestion due to nasal septal deviation who had no middle ear pathology did not change the middle ear pressure and Eustachian tube function after 3-6 months. Finally, based on this study and similar studies, it can be concluded that septoplasty surgery does not have a significant effect on Eustachian tube function and middle ear pressure, and septoplasty surgery is not necessary before ear surgeries such as tympanoplasty.
Acknowledgements: None declared by the authors.
Ethical Permission: This study was conducted after approval by the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.1292) and in coordination with the officials of Sina and Imam Reza hospitals.
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
References
1. Marino MJ, Ling LC, Yao WC, Luong A, Citardi MJ. Eustachian tube dysfunction symptoms in patients treated in a tertiary rhinology clinic. Int Forum Allergy Rhinol. 2017;7(12):1135-9. [Link] [DOI:10.1002/alr.22030]
2. Tangbumrungtham N, Patel VS, Thamboo A, Patel ZM, Nayak JV, Ma Y. The prevalence of Eustachian tube dysfunction symptoms in patients with chronic rhinosinusitis. Int Forum Allergy Rhinol. 2018;8(5):620-3. [Link] [DOI:10.1002/alr.22056]
3. Roeyen SV, Heyning PV, Rompaey VV. Value and discriminative power of the seven-item eustachian tube dysfunction questionnaire. Laryngoscope. 2015;125(11):2553-6. [Link] [DOI:10.1002/lary.25316]
4. Maniakas A, Desrosiers M, Asmar MH, Al Falasi M, Endam LM, Hopkins C, et al. Eustachian tube symptoms are frequent in chronic rhinosinusitis and respond well to endoscopic sinus surgery. Rhinology. 20181;56(2):118-21. [Link] [DOI:10.4193/Rhin17.165]
5. Hong SN, Lee WH, Lee SH, Rhee CS, Lee CH, Kim JH, et al. Chronic rhinosinusitis with nasal polyps is associated with chronic otitis media in the elderly. Eur Arch Otorhinolaryngol. 2017;274(3):1463-70. [Link] [DOI:10.1007/s00405-016-4363-0]
6. Smith ME, Takwoingi Y, Deeks J, Alper C, Bance ML, Bhutta MF. Eustachian tube dysfunction: A diagnostic accuracy study and proposed diagnostic pathway. PLoS One. 2018;13(11):e0206946. [Link] [DOI:10.1371/journal.pone.0206946]
7. Han WG, Yoo J, Rah YC, Chang J, Im GJ, Song JJ, et al. Analysis of Eustachian Tube Dysfunction by dynamic slow motion video endoscopy and eustachian tube dysfunction questionnaire in chronic otitis media. Clin Exp Otorhinolaryngol. 2017;10(4):315-20. [Link] [DOI:10.21053/ceo.2016.01683]
8. Kaya M, Dağlı E, Kırat S. Does nasal septal deviation affect the eustachian tube function and middle ear ventilation? Turk Arch Otorhinolaryngol. 2018;56(2):102-5. [Link] [DOI:10.5152/tao.2018.2671]
9. Doğan R. The effect of types of nasal septum deviation on the eustachian tube function. Bezmialem Sci. 219;7(1):33-7. [Link] [DOI:10.14235/bas.galenos.2017.2285]
10. Kishimoto H, Matsuura Y, Kawai K, Yamada S, Suzuki S. The lesser palatine nerve innervates the levator veli palatini muscle. Plast Reconstr Surg Glob Open. 2016;4(9):e1044. [Link] [DOI:10.1097/GOX.0000000000001044]
11. Vila PM, Thomas T, Liu C, Poe D, Shin JJ. The burden and epidemiology of eustachian tube dysfunction in adults. Otolaryngol Head Neck Surg. 2017;156(2):278-84. [Link] [DOI:10.1177/0194599816683342]
12. Shan A, Ward BK, Goman AB, Betz JF, Reed NS, Poe DS, et al. prevalence of eustachian tube dysfunction in adults in the united states. JAMA Otolaryngol Head Neck Surg. 2019; 145(10): 974-5. [Link] [DOI:10.1001/jamaoto.2019.1917]
13. Schilder AG, Bhutta MF, Butler CC, Holy C, Levine LH, Kvaerner KJ, et al. Eustachian tube dysfunction: Consensus statement on definition, types, clinical presentation and diagnosis. Clin Otolaryngol. 2015;40(5):407-11. [Link] [DOI:10.1111/coa.12475]
14. Huisman JML Verdam FJ, Stegeman I, Ru JA. Treatment of Eustachian tube dysfunction with balloon dilation: A systematic review. Laryngoscope. 2018;128(1):237-47. [Link] [DOI:10.1002/lary.26800]
15. Meyer TA, O'Malley EM, Schlosser RJ, Soler ZM, Cai J, Hoy MJ, et al. A randomized controlled trial of balloon dilation as a treatment for persistent eustachian tube dysfunction with 1-year follow-up. Otol Neurotol. 2018 ;39(7):894-902. [Link] [DOI:10.1097/MAO.0000000000001853]
16. Poe D, Anand V, Dean M, Roberts WH, Stolovitzky JP, Hoffmann K, et al. Balloon dilation of the eustachian tube for dilatory dysfunction: A randomized controlled trial. Laryngoscope. 2018;128(5):1200-6. [Link] [DOI:10.1002/lary.26827]
17. Luukkainen V, Kivekäs I, Silvola J, Jero J, Sinkkonen ST. Balloon eustachian tuboplasty: Systematic review of long-term outcomes and proposed indications. J Int Adv Otol. 2018;14(1):112-26. [Link] [DOI:10.5152/iao.2018.4769]
18. Roeyen SV, Heyning PV, Rompaey VV. responsiveness of the 7-item eustachian tube dysfunction questionnaire. J Int Adv Otol. 2016;12(1):106-8. [Link] [DOI:10.5152/iao.2016.2086]
19. Meyer MF, Korthäuer C, Jansen S, Hüttenbrink KB, Beutner D. Analyzing eustachian tube function in patients with symptoms of chronical Eustachian tube dysfunction by pressure chamber measurements. Eur Arch Otorhinolaryngol. 2018;275(5):1087-94. [Link] [DOI:10.1007/s00405-018-4938-z]
20. Akyildiz MY, Özmen OA, Demir UL, Kasapoğlu F, Coşkun HH, Basut OI, et al. Impact of septoplasty on eustachian tube functions. J Craniofac Surg. 2017;28(8):1929-32. [Link] [DOI:10.1097/SCS.0000000000003927]