GMJ Medicine
eISSN : 2626-3041
Volume 2, Issue 3 (2023)
GMJM 2023, 2(3): 87-90 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/12/24 | Accepted: 2023/08/5 | Published: 2023/09/17
Received: 2022/12/24 | Accepted: 2023/08/5 | Published: 2023/09/17
How to cite this article
Maroufi P, Nazari B. Relationship Between Bone Density and Hip Fractures. GMJM 2023; 2 (3) :87-90
URL: http://gmedicine.de/article-2-204-en.html
URL: http://gmedicine.de/article-2-204-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
P. Maroufi1, B. Nazari *2
1- Department of Orthopedics, School of Medicine, Shohada Medical Research & Training Hospital, Tabriz University of Medical Sciences, Tabriz, Iran
2- Department of Orthopedics, School of Medicine, Rahat Breath and Sleep Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2- Department of Orthopedics, School of Medicine, Rahat Breath and Sleep Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Keywords:
| Abstract (HTML) (1525 Views)
Full-Text: (356 Views)
Introduction
The incidence of hip fractures has been increasing in recent years, so that it can be said that 40% of women over the age of 50 experience this fracture at least once [1]. The mortality rate due to hip fracture is about 20%, which is much higher compared to other orthopedic diseases (less than 1%) [2] (Figure 1).
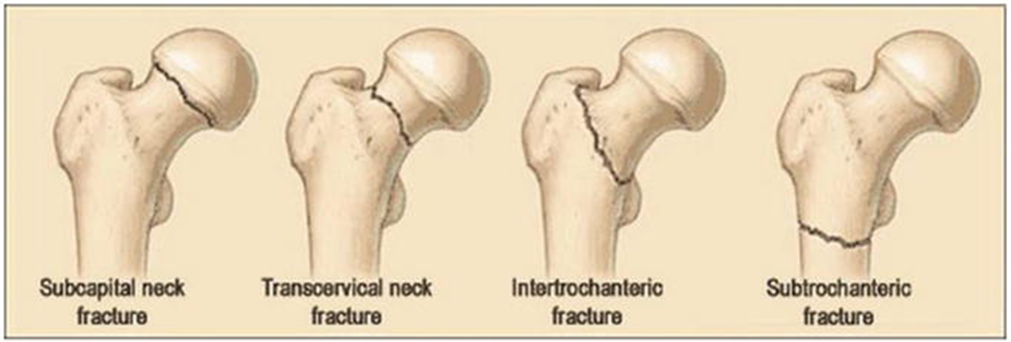
Figure 1) Hip Fracture: Anatomy, Causes, and Consequences
Most people will develop osteoporosis in old age, but in women, osteoporosis may even begin before menopause; However, fractures occur at an older age [3]. Menopausal women are most likely to be at risk for osteoporotic fractures; Because estrogen levels are significantly reduced during this period. Hip fractures are the most serious complication of osteoporosis, or osteoporosis, which occurs in three-quarters of Hip fractures in women. If we measure bone mineral density, a significant number of women, especially during menopause, suffer from a decrease in bone mass in the neck and femur [4].
In addition to the risk of death, patients with hip fractures are at risk for many other problems, including deep vein thrombosis, bed sores, and urinary tract infections. Although several factors are involved in causing Hip fractures, osteoporosis has been suggested as the most important cause of Hip fractures [5].
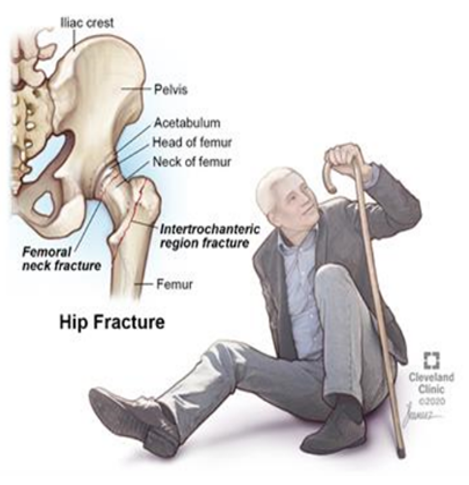
Figure 2) Hip Fracture & Broken Hip
There are several methods for determining bone density, including Radiographic Absorptiometry, Ultrasound, Quantitative CT, and Dual-Energy X-ray Absorptiometry. However, the method of determining bone density by Dual-Energy X-ray Absorptiometry is considered as the gold standard [6, 7].
As mentioned, although osteoporosis has been mentioned as the most important cause of Hip fractures, so far very limited studies have been performed to determine the level of osteoporosis that leads to fractures, which is an important issue in this article; Therefore, the aim of this study was to determine the relationship between bone density and the risk of hip fracture (Figure 2).
Materials and Methods
This descriptive-analytical study was performed with the participation of 200 participants (100 patients and 100 healthy individuals) in the orthopedic hospital of Tabriz University of Medical Sciences. Patients with hip fractures were assessed for bone mineral density by Dual-Energy X-ray Absorptiometry and their bone mineral density was compared with that of healthy individuals. in 100 patients (50 men, 50 women) who had hip fractures following minor trauma. The age of patients was between 50 and 90 years. To prevent osteoporosis due to immobilization, all measurements were taken within the first two weeks after the fracture. In order to prevent laboratory error, all measurements were performed on the healthy side of the patient.
The control group consisted of 100 people (50 females, 50 males) aged between 50 and 90 years. The control group was selected from the normal population so that these individuals had never had a Hip fracture. In these patients, hip bone density was measured by Dual-Energy X-ray Absorptiometry. All measurements were performed by a specific technician. The following items were excluded from the study to avoid research errors:
1. Patients with impaired bone metabolism;
2. Patients who had had a Hip fracture for more than two weeks;
3. Patients who developed osteoporosisdue to medication;
4. Patients with fractures following severe trauma; and
5. Patients who had a previous fracture or previous surgery at the site of a hip fracture.
In measuring the density of bone by Dual-Energy X-ray Absorptiometry, each person (patient or healthy person) has three indicators:
Indicator 1: The amount of bone density, which actually indicates the mineral content of bone, which is expressed in grams per cubic centimeter.
Indicator 2: T index, which is a comparison between the bone density of each person with a young person.
Indicator 3: Z index, which is a comparison between the bone density of each person with a person of the same age and gender.
The collected data were entered into SPSS 20 software and displayed using number and percentage, mean and standard deviation; T-test was also used to compare the results.
No additional costs were incurred by the patients and the patients entered the study after signing a written informed consent. The objectives of the study were explained to all participants in simple language to enter the study with full knowledge.
Findings
The mean age of participants in the group of patients was 71.49±5.69 years and in the group of healthy individuals was 69.34±5.29 years (p=0.254). The history of hypertension (p=0.045), diabetes (p=0.036), previous history of bone fractures (p=0.001) and smoking (p=0.037) were significantly higher in patients group than healthy individuals.
The mean of bone density in the patient group (0.6254g/cm3; Max 1/Min 0.225) was significantly (p=0.003) lower than the control group (0.8145g/cm3; Max 1.214/Min 0.457).
The mean of T-index in the patient group (-2.645; Max 4.4/Min 1.7) was significantly (p=0.001) lower than the control group (-14.1; Max 4.5/Min 0.7).
The mean of Z index in the patient group (-1.125; Max 1.3/Min 0.5) was significantly (p=0.001) lower than the control group (-0.445; Max 2.1/Min 0.5).
The bone density in elderly patients had positive relationships with the history of hypertension (p=0.045), history of diabetes (p=0.014), history of previous bone fractures (p=0.001) and smoking (p=0.019). The T-index in elderly patients had positive relationships with the history of hypertension (p=0.048), history of diabetes (p=0.037), previous history of bone fractures (p=0.001) and smoking (p=0.017). The Z-index in elderly patients had positive relationships with the history of hypertension (p=0.049), history of diabetes (p=0.041), previous history of bone fractures (p=0.001) and smoking (p=0.027).
Discussion
Osteoporosis causes bones to become weak and brittle. So much so that even a simple fall or slight pressure on the bone when coughing can cause it to break. Fractures due to osteoporosis mainly occur in the bones of the pelvis, wrist or spine. Bone is a living tissue whose structure is constantly decomposing and replacing [8-10]. Osteoporosis occurs when the rate of production of new bone is slower than the rate of loss of old tissue. Osteoporosis can affect both men and women of all races. Taking the right medications, eating a healthy and nutritious diet, and doing aerobic exercise to strengthen the body's weight-bearing organs can help prevent osteoporosis or strengthen weakened bones [11].
Fractures due to osteoporosis are often caused by very common events that healthy people will never fracture in those situations. Examples include vertebral fractures, many of which occur with a slight pressure such as lifting an object, sneezing, and bending. If the underlying cause for osteoporosis is diagnosed, it will be done. The diagnosis of osteoporosis is usually made by a bone density test and is usually performed at an older age [12]. Bone mineral density measurements are usually requested by a specialist at an advanced age or following an acute fracture. Radiographs will not be a good indicator of osteoporosis; Because too little or too much radiation penetrates the photographic film, it affects its quality and impairs the detection. The best way to diagnose osteoporosis is to measure bone mineral density [13].
The financial burden of fractures and osteoporosis in Iran is very high and this figure is estimated at more than 3 thousand billion tomans annually. About 50% of this figure is related to the incidence of fractures due to osteoporosis, which is a very high figure. The incidence of pelvic fractures is 157 per 100,000 among Iranian women and 138 per 100,000 among men, which indicates that bone fractures are very high in Iran. Fifty percent of pelvic fractures occur in people who have experienced a fracture once. If these people are identified and treated in time, a significant percentage of fractures will be reduced [14].
Bone density measurement or bone densitometry is the name of a method that can be used to determine the stiffness and degree of strength of the bones in the body. There are different ways to measure bone density, but the most common is DEXA, which stands for Dual Energy X-ray Absorptiometry, which uses X-rays to measure bone density. In this method, X-rays are sent to the bone from two sources to measure its density. Some of the radiation is absorbed by the bone and some of it passes through the bone and leaves the other side of the body. The amount of each of these two rays is measured by a receptor after leaving the body [15, 16]. The higher the bone density (meaning that there are fewer pores and small spaces inside the bone), the more X-rays it absorbs, the less radiation it allows to pass through, and the less radiation reaches the recipient [17 ,18]. The received radiation is sent to a computer by the receiver or detector, where the scale of the amount of radiation is converted to the scale of bone density. Use two X-ray sources to make the measurement more accurate. The gold standard in the diagnosis of osteoporosis is the use of bone mineral density, which in this study proved its positive and confirmatory effects [19, 20].
Failure to enter the degree of fracture in patients, lack of information about the supplements taken by patients, lack of knowledge about the last menopause of women and also lack of knowledge about the family history of bone problems such as osteoporosis were the limitations of this study. These problems will be solved in the future.
Conclusion
Osteoporosis is the leading cause of fractures in the elderly, and factors such as a history of bone fractures, old age, diabetes and high blood pressure, as well as smoking can increase its severity. The gold standard for diagnosing this problem is measuring bone density.
Acknowledgements: None declared by the authors.
Ethical Permission: This study has been approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1399.477).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
The incidence of hip fractures has been increasing in recent years, so that it can be said that 40% of women over the age of 50 experience this fracture at least once [1]. The mortality rate due to hip fracture is about 20%, which is much higher compared to other orthopedic diseases (less than 1%) [2] (Figure 1).
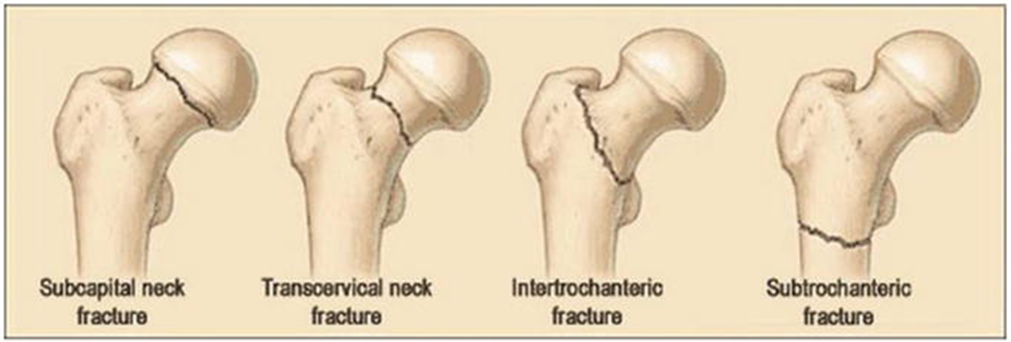
Figure 1) Hip Fracture: Anatomy, Causes, and Consequences
Most people will develop osteoporosis in old age, but in women, osteoporosis may even begin before menopause; However, fractures occur at an older age [3]. Menopausal women are most likely to be at risk for osteoporotic fractures; Because estrogen levels are significantly reduced during this period. Hip fractures are the most serious complication of osteoporosis, or osteoporosis, which occurs in three-quarters of Hip fractures in women. If we measure bone mineral density, a significant number of women, especially during menopause, suffer from a decrease in bone mass in the neck and femur [4].
In addition to the risk of death, patients with hip fractures are at risk for many other problems, including deep vein thrombosis, bed sores, and urinary tract infections. Although several factors are involved in causing Hip fractures, osteoporosis has been suggested as the most important cause of Hip fractures [5].
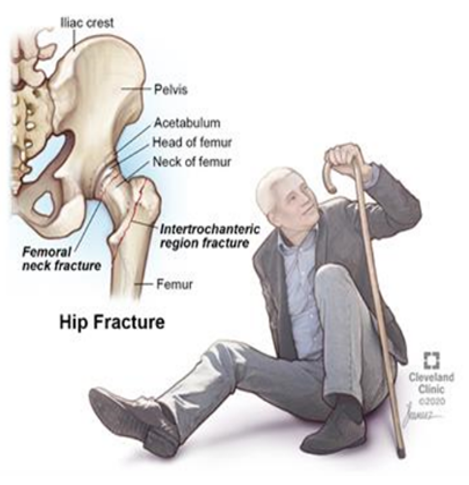
Figure 2) Hip Fracture & Broken Hip
There are several methods for determining bone density, including Radiographic Absorptiometry, Ultrasound, Quantitative CT, and Dual-Energy X-ray Absorptiometry. However, the method of determining bone density by Dual-Energy X-ray Absorptiometry is considered as the gold standard [6, 7].
As mentioned, although osteoporosis has been mentioned as the most important cause of Hip fractures, so far very limited studies have been performed to determine the level of osteoporosis that leads to fractures, which is an important issue in this article; Therefore, the aim of this study was to determine the relationship between bone density and the risk of hip fracture (Figure 2).
Materials and Methods
This descriptive-analytical study was performed with the participation of 200 participants (100 patients and 100 healthy individuals) in the orthopedic hospital of Tabriz University of Medical Sciences. Patients with hip fractures were assessed for bone mineral density by Dual-Energy X-ray Absorptiometry and their bone mineral density was compared with that of healthy individuals. in 100 patients (50 men, 50 women) who had hip fractures following minor trauma. The age of patients was between 50 and 90 years. To prevent osteoporosis due to immobilization, all measurements were taken within the first two weeks after the fracture. In order to prevent laboratory error, all measurements were performed on the healthy side of the patient.
The control group consisted of 100 people (50 females, 50 males) aged between 50 and 90 years. The control group was selected from the normal population so that these individuals had never had a Hip fracture. In these patients, hip bone density was measured by Dual-Energy X-ray Absorptiometry. All measurements were performed by a specific technician. The following items were excluded from the study to avoid research errors:
1. Patients with impaired bone metabolism;
2. Patients who had had a Hip fracture for more than two weeks;
3. Patients who developed osteoporosisdue to medication;
4. Patients with fractures following severe trauma; and
5. Patients who had a previous fracture or previous surgery at the site of a hip fracture.
In measuring the density of bone by Dual-Energy X-ray Absorptiometry, each person (patient or healthy person) has three indicators:
Indicator 1: The amount of bone density, which actually indicates the mineral content of bone, which is expressed in grams per cubic centimeter.
Indicator 2: T index, which is a comparison between the bone density of each person with a young person.
Indicator 3: Z index, which is a comparison between the bone density of each person with a person of the same age and gender.
The collected data were entered into SPSS 20 software and displayed using number and percentage, mean and standard deviation; T-test was also used to compare the results.
No additional costs were incurred by the patients and the patients entered the study after signing a written informed consent. The objectives of the study were explained to all participants in simple language to enter the study with full knowledge.
Findings
The mean age of participants in the group of patients was 71.49±5.69 years and in the group of healthy individuals was 69.34±5.29 years (p=0.254). The history of hypertension (p=0.045), diabetes (p=0.036), previous history of bone fractures (p=0.001) and smoking (p=0.037) were significantly higher in patients group than healthy individuals.
The mean of bone density in the patient group (0.6254g/cm3; Max 1/Min 0.225) was significantly (p=0.003) lower than the control group (0.8145g/cm3; Max 1.214/Min 0.457).
The mean of T-index in the patient group (-2.645; Max 4.4/Min 1.7) was significantly (p=0.001) lower than the control group (-14.1; Max 4.5/Min 0.7).
The mean of Z index in the patient group (-1.125; Max 1.3/Min 0.5) was significantly (p=0.001) lower than the control group (-0.445; Max 2.1/Min 0.5).
The bone density in elderly patients had positive relationships with the history of hypertension (p=0.045), history of diabetes (p=0.014), history of previous bone fractures (p=0.001) and smoking (p=0.019). The T-index in elderly patients had positive relationships with the history of hypertension (p=0.048), history of diabetes (p=0.037), previous history of bone fractures (p=0.001) and smoking (p=0.017). The Z-index in elderly patients had positive relationships with the history of hypertension (p=0.049), history of diabetes (p=0.041), previous history of bone fractures (p=0.001) and smoking (p=0.027).
Discussion
Osteoporosis causes bones to become weak and brittle. So much so that even a simple fall or slight pressure on the bone when coughing can cause it to break. Fractures due to osteoporosis mainly occur in the bones of the pelvis, wrist or spine. Bone is a living tissue whose structure is constantly decomposing and replacing [8-10]. Osteoporosis occurs when the rate of production of new bone is slower than the rate of loss of old tissue. Osteoporosis can affect both men and women of all races. Taking the right medications, eating a healthy and nutritious diet, and doing aerobic exercise to strengthen the body's weight-bearing organs can help prevent osteoporosis or strengthen weakened bones [11].
Fractures due to osteoporosis are often caused by very common events that healthy people will never fracture in those situations. Examples include vertebral fractures, many of which occur with a slight pressure such as lifting an object, sneezing, and bending. If the underlying cause for osteoporosis is diagnosed, it will be done. The diagnosis of osteoporosis is usually made by a bone density test and is usually performed at an older age [12]. Bone mineral density measurements are usually requested by a specialist at an advanced age or following an acute fracture. Radiographs will not be a good indicator of osteoporosis; Because too little or too much radiation penetrates the photographic film, it affects its quality and impairs the detection. The best way to diagnose osteoporosis is to measure bone mineral density [13].
The financial burden of fractures and osteoporosis in Iran is very high and this figure is estimated at more than 3 thousand billion tomans annually. About 50% of this figure is related to the incidence of fractures due to osteoporosis, which is a very high figure. The incidence of pelvic fractures is 157 per 100,000 among Iranian women and 138 per 100,000 among men, which indicates that bone fractures are very high in Iran. Fifty percent of pelvic fractures occur in people who have experienced a fracture once. If these people are identified and treated in time, a significant percentage of fractures will be reduced [14].
Bone density measurement or bone densitometry is the name of a method that can be used to determine the stiffness and degree of strength of the bones in the body. There are different ways to measure bone density, but the most common is DEXA, which stands for Dual Energy X-ray Absorptiometry, which uses X-rays to measure bone density. In this method, X-rays are sent to the bone from two sources to measure its density. Some of the radiation is absorbed by the bone and some of it passes through the bone and leaves the other side of the body. The amount of each of these two rays is measured by a receptor after leaving the body [15, 16]. The higher the bone density (meaning that there are fewer pores and small spaces inside the bone), the more X-rays it absorbs, the less radiation it allows to pass through, and the less radiation reaches the recipient [17 ,18]. The received radiation is sent to a computer by the receiver or detector, where the scale of the amount of radiation is converted to the scale of bone density. Use two X-ray sources to make the measurement more accurate. The gold standard in the diagnosis of osteoporosis is the use of bone mineral density, which in this study proved its positive and confirmatory effects [19, 20].
Failure to enter the degree of fracture in patients, lack of information about the supplements taken by patients, lack of knowledge about the last menopause of women and also lack of knowledge about the family history of bone problems such as osteoporosis were the limitations of this study. These problems will be solved in the future.
Conclusion
Osteoporosis is the leading cause of fractures in the elderly, and factors such as a history of bone fractures, old age, diabetes and high blood pressure, as well as smoking can increase its severity. The gold standard for diagnosing this problem is measuring bone density.
Acknowledgements: None declared by the authors.
Ethical Permission: This study has been approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1399.477).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
References
1. Singer A, Exuzides A, Spangler L, O'Malley C, Colby C, Johnston K, et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90(1):53-62. [Link] [DOI:10.1016/j.mayocp.2014.09.011]
2. Walker J, Tucker LY, Goodney P, Candell L, Hua H, Okuhn S, et al. Type II endoleak with or without intervention after endovascular aortic aneurysm repair does not change aneurysm-related outcomes despite sac growth. J Vasc Surg. 2015;62(3):551-61. [Link] [DOI:10.1016/j.jvs.2015.04.389]
3. Abrahamsen B, Eiken P, Prieto-Alhambra D. Risk of hip, subtrochanteric, and femoral shaft fractures among mid and long term users of alendronate: Nationwide cohort and nested case-control study. BMJ Clin Res. 2016; 353:i3365. [Link] [DOI:10.1136/bmj.i3365]
4. Adams AL, Shi JM, Reynolds K, Haque R, Cheetham TC, Kawatkar AA, et al. Statins and hip fracture risk in men: A population-based case-control study. 2015;25(11):844-8. [Link] [DOI:10.1016/j.annepidem.2015.08.010]
5. Karakatsani A, Katsoulis M, Klinaki E, Trichopoulou A. Corticosteroids and hip fracture risk in elderly respiratory patients: EPIC-Greece cohort. Adv Respir Med. 2017;85(1):22-27. [Link] [DOI:10.5603/ARM.2017.0005]
6. Thaler HW, Sterke CS, van der Cammen TJ. Association of proton pump inhibitor use with recurrent falls and risk of fractures in older women: A study of medication use in older fallers. J Nutr Health Aging. 2016;20(1):77-81. [Link] [DOI:10.1007/s12603-016-0679-0]
7. Ward IM, Mortensen EM, Battafarano DF, Frei CR, Mansi I. Association of statins and risk of fractures in a military health system: A propensity score-matched analysis. Ann Pharmacother. 2014;48(11):1406-14. [Link] [DOI:10.1177/1060028014545038]
8. Milovanovic DR, Pirkovic MS, Simonovic SZ, Matovic M, Dejanovic SD, Jankovic SM, et al. Parameters of calcium metabolism fluctuated during initiation or changing of antipsychotic drugs. Psychiatry Investig. 2016;13(1):89-101. [Link] [DOI:10.4306/pi.2016.13.1.89]
9. Xiao X, Xu Y, Wu Q. Thiazide diuretic usage and risk of fracture: A meta-analysis of cohort studies. Osteoporos Int. 2018;29(7):1515-24. [Link] [DOI:10.1007/s00198-018-4486-9]
10. Hughes JM, McKinnon CJ, Taylor KM, Kardouni JR, Bulathsinhala L, Guerriere KI, et al. Nonsteroidal anti-inflammatory drug prescriptions are associated with increased stress fracture diagnosis in the US army population. J Bone Miner Res. 2019;34(3):429-36. [Link] [DOI:10.1002/jbmr.3616]
11. Zhao JG, Zeng XT, Wang J, Liu L. Association between Calcium or Vitamin D supplementation and fracture incidence in community-dwelling older adults: A systematic review and meta-analysis. JAMA. 2017;318(24):2466-82. [Link] [DOI:10.1001/jama.2017.19344]
12. Yao P, Bennett D, Mafham M, Lin X, Chen Z, Armitage J, et al. Vitamin D and Calcium for the prevention of fracture: A systematic review and meta-analysis. JAMA Netw Open. 2019;2(12):e1917789. [Link] [DOI:10.1001/jamanetworkopen.2019.17789]
13. Cram P, Yan L, Bohm E, Kuzyk P, Lix LM, Morin SN, et al. Trends in operative and nonoperative hip fracture management 1990-2014: A longitudinal analysis of manitoba administrative data. J Am Geriatr Soc. 2017;65(1):27-34. [Link] [DOI:10.1111/jgs.14538]
14. Kang Y, Liu J, Chen H, Ding W, Chen J, Zhao B, et al. Enhanced recovery after surgery (ERAS) in elective intertrochanteric fracture patients result in reduced length of hospital stay (LOS) without compromising functional outcome. J Orthop Surg Res. 20199;14(1):209. [Link] [DOI:10.1186/s13018-019-1238-2]
15. Vannucci L, Brandi ML. Healing of the bone with anti-fracture drugs. Expert Opin Pharmacother. 2016;17(17):2267-72. [Link] [DOI:10.1080/14656566.2016.1241765]
16. Huang TW, Chuang PY, Lin SJ, Lee CY, Huang KC, Shih HN, et al. Teriparatide improves fracture healing and early functional recovery in treatment of osteoporotic intertrochanteric fractures. Medicine (Baltimore). 2016;95(19):e3626. [Link] [DOI:10.1097/MD.0000000000003626]
17. Huang TW, Yang TY, Huang KC, Peng KT, Lee MS, Hsu RW. Effect of teriparatide on unstable pertrochanteric fractures. Biomed Res Int. 2015;2015:568390. [Link] [DOI:10.1155/2015/568390]
18. Bhandari M, Jin L, See K, Burge R, Gilchrist N, Witvrouw R, et al. Does teriparatide improve femoral neck fracture healing: Results from a randomized placebo-controlled trial. Clin Orthop Relat Res. 2016;474(5):1234-44. [Link] [DOI:10.1007/s11999-015-4669-z]
19. Kim SJ, Park HS, Lee DW, Lee JW. Does short-term weekly teriparatide improve healing in unstable intertrochanteric fractures?. J Orthop Surg (Hong Kong). 2018;26(3):2309499018802485. [Link] [DOI:10.1177/2309499018802485]
20. Li Q, Ke C, Han S, Xu X, Cong YX, Shang K, et al. Nonoperative treatment versus volar locking plate fixation for elderly patients with distal radial fracture: A systematic review and meta-analysis. J Orthop Surg Res. 2020;15(1):263. [Link] [DOI:10.1186/s13018-020-01734-2]