GMJ Medicine
eISSN : 2626-3041
Volume 3, Issue 3 (2024)
GMJM 2024, 3(3): 103-106 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2023/12/28 | Accepted: 2024/06/21 | Published: 2024/08/8
Received: 2023/12/28 | Accepted: 2024/06/21 | Published: 2024/08/8
How to cite this article
Tabibzadeh Dezfuli S, Ghasemi H, Yazdani R. Accuracy of Rapid Ultrasound in Shock on Detection of Early Rapid Shock Type in Emergency Patients. GMJM 2024; 3 (3) :103-106
URL: http://gmedicine.de/article-2-239-en.html
URL: http://gmedicine.de/article-2-239-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Trauma and Emergency Medicine Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
2- Emergency Medicine Specialist, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
2- Emergency Medicine Specialist, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
Keywords:
| Abstract (HTML) (1777 Views)
Full-Text: (537 Views)
Introduction
Shock includes conditions that threatens life and is divided into four categories including cardiogenic, hypovolemic, distributive and obstructive [1]. Some shocks such as accidents have interested different individuals [2]. Since different shocks need special treatments, it is needed to use quick-detection techniques for recognition of shock in the emergency department and critical care units [2]. The detection of cause of shock is conducted by using history of the patients and laboratory tests, but there may be errors for accuracy of emergency tests [3].
For several years, shock detection techniques have been used on the basis of ultrasound technology [4]. Abdominal and cardiac evaluation in life support, rapid ultrasound in shock (RUSH), critical care ultrasonography and echocardiography guided life support are commonly used [5]. The use of ultrasound in patients with undifferentiated shock helps rapid evaluation and early in undifferentiated hypotension [6]. Early and accuracy recognition of shock can reduce mortality [7, 8]. The RUSH is a novel emergency ultrasound protocol that uses pulmonary assessment with cardiac, abdominal, and venous evaluation [9-11]. The RUSH protocol are consisted from three stages with different factors including Tank, Pipe and Pump [5]. This technique investigates Pump’s anatomy of the heart cavity, mechanical stresses on it and the cardiac contractile power and the obstructive condition of cardiac output like cardiac tamponed and Massive pulmonary emboli [12].
A study reported an appropriate Kappa correlation coefficient by 0.84 for comparison of RUSH technique and final diagnosis that show efficiency of the protocol. They also reported sensitivity of 88% and specificity of 96%. In the study mentioned, recognition was correctly conducted for 81% patients [13]. Other study reported Kappa’s correlation coefficient of 0.7 for RUSH [14]. Previous studies have suggested using protocol for better and faster diagnosis [9]. RUSH technique is one of protocols used for early diagnosis and continuous monitoring of patients in emergency departments [11, 15].
There was need to conduct a study for evaluation of accuracy of RUSH in early recognition of emergency department patients. This study was thus conducted to investigate accuracy of RUSH in early recognition of emergency department patients.
Materials and Methods
Patients
A case-control study was conducted in the emergency department of Shahid Mohammadi hospital for detecting accuracy of the RUSH technique. It was approved by the ethics committee of Hormozgan University of Medical Sciences.
Participants
During April 2016 to May 2017, we have recorded all the patients with shock at the emergency department of Shahid Mohammadi hospital and the samples were selected by simple sampling method. On the basis of the time of the patients’ arrival, the emergency physicians or radiologist conducted the sonography exams on the basis of the RUSH procedure concurrent with ongoing care of each patient.
Shock classification and rapid ultrasound in shock protocol
In the current study shock was classified into 4 groups: hypovolemic, cardiogenic, distributive (septic or neurogenic) and obstructive (due to pneumothorax, tamponade, pulmonary thromboembolic disease). Some patients showed a combination of shocks and grouped as mixed type. Some components are used in RUSH exam including evaluation of inferior vena cava, thoracic and abdominal compartments and large arteries and veins. Pericardial effusion, cardiac tamponade, ascite, pleural effusion and pulmonary edema were investigated.
Statistical Analysis
SPSS 20 software was used for analyzing the data. We have evaluated the overall agreement of defined shock types on the basis of RUSH results and final diagnosis of patients via calculating the Kappa index. Subgroup analysis and investigation of Kappa index for results of the RUSH exam were used. The Kappa agreement and reliability indices sensitivity, specificity, positive (PPV) and negative predictive values (NPV) were used.
Findings
Demographic and clinical characteristics
The mean age was 64.04±9.2 (45 to 86) years. Out of 52 patients studied, pulmonary and cardiac signs were as follows; 21 patients with pericardial effusion (40.4%), 9 patients with cardiac tamponade (17.3%), 25 patients with ascite (48.1%), 25 patients with ascite (48.1%), 25 patients with pleural effusion (48.1%) and 18 patients with pulmonary edema (34.6%).
Prevalence of different types of shock
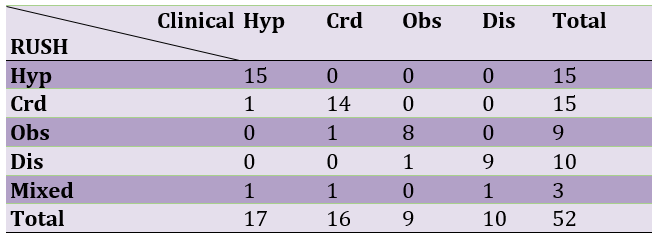
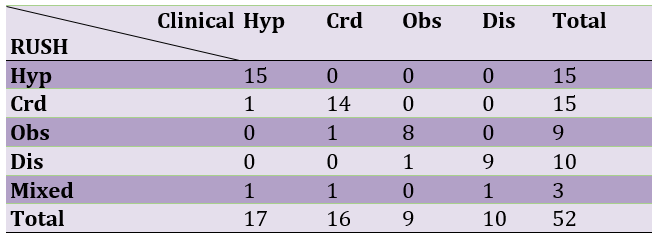
On the basis the procedures, hypovolemic and cardiogenic shocks had most frequent among types of shock (Table 1).
Table 1. Prevalence of hypovolemic (Hyp), cardiogenic (Crd), obstructive (Obs), and distributive (Dis) shock based on final clinical diagnosis and RAUSH exam
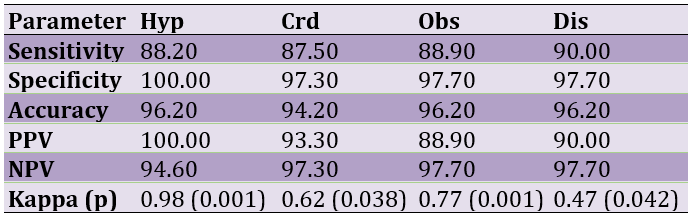
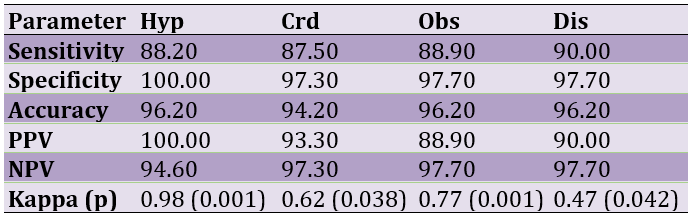
The data for accuracy, sensitivity, specificity, PPV, NPV and Kappa index of the protocol for type of shock are shown in Table 2. The results for Kappa index for general agreement between shock types was defined by the RUSH protocol and final diagnosis was 0.85 (p=0.001) for all patients.
Table 2. Reliability indices and Kappa agreement of the rapid ultrasound in shock exam for hypovolemic (Hyp), cardiogenic (Crd), obstructive (Obs), and distributive (Dis) shock
Hypovolemic Shock
The data for hypovolemic shock showed good sensitivity, excellent agreement, specificity and accuracy and highest agreement with final diagnoses were observed for this shock. We had 15 cases finally diagnosed as having hypovolemic shocks who were all observed on the basis of RUSH findings (88.2% sensitivity, and 100% PPV). In the current study, among 17 diagnosed, 15 patients were correctly diagnosed, 1 patient was diagnosed in cardiogenic shock and 1 patient in mixed shock.
Cardiogenic shock
Good sensitivity, excellent specificity, accuracy and agreement were observed for cardiogenic shock. We have correctly distinguished 14 out of 16 cardiogenic shock cases, indicating good sensitivity (87.50%). Other patients were diagnosed as obstructive and mixed respectively. The results showed 87.5%, 97.3%, 94.2%, 93.3%, 97.3% and 0.62 for sensitivity, specificity, accuracy, PPV, NPV and agreement respectively.
Obstructive Shock
The data for obstructive shock showed good sensitivity and agreement, excellent specificity and accuracy. We had 10 cases finally diagnosed as having obstructive shocks in which 9 patients were diagnosed as obstructive on the basis of RUSH findings (96.2% accuracy, and 88.9% PPV). In the current study, other patient was diagnosed as distributive. The results showed 88.9%, 97.7%, 96.2%, 88.9%, 97.7% and 0.77 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively.
Distributive shock
Low agreement, excellent specificity, sensitivity and accuracy were seen in distributive shock. We have found 10 patients with distributive shocks with the early RUSH exam that 9 patients belonged to this shock, showing good sensitivity. The results showed 90.0%, 97.7%, 96.2%, 90.0%, 97.7% and 0.47 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively.
PPV, positive predictive value of RUSH criteria to determine each type of shock; NPV, negative predictive value of RUSH criteria to determine each shock type; Kappa, index of agreement between diagnosis of shock type based on RUSH criteria and final diagnosis.
Discussion
Shock includes conditions that threatens life and is divided into four categories including cardiogenic, hypovolemic, distributive and obstructive [1]. Since different shocks need special treatments, it is needed to use quick-detection techniques for recognition of shock in the emergency department and critical care units [2]. The results showed an acceptable appropriate agreement between the results obtained and final clinical diagnosis of patients (Kappa=0.85). Some fast protocols are increasingly in access for providing associated information to the pathology and management of shocks condition. The RUSH protocol has advantages including learning doing, the simple equipment needed, simplicity and a possible direct vision of volume. A study reported similar agreement for their study that focused on a similar multi-organ sonography assessment of emergency patients [16]. Bagheri Hariri et al. [17] reported Kappa correlation coefficient for comparison of the RUSH technique and the final diagnosis by 0.84% that shows a high compliance rate of the protocol. Another study reported Kappa’s correlation coefficient for comparison of the RUSH by 0.85 [12].
The results show that use of RUSH is appropriate option for early recognition in patients with shock. The RUSH technique is reliable for hypovolemic, cardiogenic or obstructive subtypes (NPV>0.94). These results show that therapeutic approaches used for treatment have appropriate effectiveness, especially for final outcome obtained. Hypovolemic shock is usually occurs due to bleeding or severe fluid loss [12]. The RUSH technique is on the basis of the hyper contractile and small chamber size for diagnosis of hypovolemic shock. The results showed 88.2%, 100%, 96.2%, 100%, 94.6% and 0.98 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively. In summary, the results showed the use of diagnostic RUSH technique in hypovolemic shock management is appropriate. Cardiogenic shock is usually occurs due to pump failure and the inappropriate ability of the heart for moving the needed oxygenated blood toward vital organs. The results showed 87.5%, 97.3%, 94.2%, 93.3%, 97.3% and 0.62 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively. Our findings confirm effectiveness of use of diagnostic RUSH technique in cardiogenic shock management is appropriate. Obstructive shock is most commonly induced through cardiac tamponade, tension pneumothorax, or largepulmonary embolus [12]. The results showed 88.9%, 97.7%, 96.2%, 88.9%, 97.7% and 0.77 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively. Overall, the results confirm effectiveness of use of diagnostic RUSH technique in obstructive shock management is appropriate. Distributive shock is most commonly induced by vascular system vasodilation in point that the core vascular blood volume is insufficient for maintaining organ perfusion [12]. This shock usually occurs following inflammation. Inflammatory response to infection increases by systemic inflammatory response syndrome (SIRS), severe sepsis and septic shock steps. The results showed 90.0%, 97.7%, 96.0%, 90.0%, 97.7% and 0.47 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively. In summary, the results showed the use of diagnostic RUSH technique in distributive shock management is appropriate.
Conclusion
In summary, the results obtained for RUSH provided reliable information for clinicians to make a fast and acceptably accurate recognition of the shock type in a hypotensive patient, especially for obstructive, cardiogenic or hypovolemic shock types.
Acknowledgments: None declared by the authors.
Ethical Permission: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Shock includes conditions that threatens life and is divided into four categories including cardiogenic, hypovolemic, distributive and obstructive [1]. Some shocks such as accidents have interested different individuals [2]. Since different shocks need special treatments, it is needed to use quick-detection techniques for recognition of shock in the emergency department and critical care units [2]. The detection of cause of shock is conducted by using history of the patients and laboratory tests, but there may be errors for accuracy of emergency tests [3].
For several years, shock detection techniques have been used on the basis of ultrasound technology [4]. Abdominal and cardiac evaluation in life support, rapid ultrasound in shock (RUSH), critical care ultrasonography and echocardiography guided life support are commonly used [5]. The use of ultrasound in patients with undifferentiated shock helps rapid evaluation and early in undifferentiated hypotension [6]. Early and accuracy recognition of shock can reduce mortality [7, 8]. The RUSH is a novel emergency ultrasound protocol that uses pulmonary assessment with cardiac, abdominal, and venous evaluation [9-11]. The RUSH protocol are consisted from three stages with different factors including Tank, Pipe and Pump [5]. This technique investigates Pump’s anatomy of the heart cavity, mechanical stresses on it and the cardiac contractile power and the obstructive condition of cardiac output like cardiac tamponed and Massive pulmonary emboli [12].
A study reported an appropriate Kappa correlation coefficient by 0.84 for comparison of RUSH technique and final diagnosis that show efficiency of the protocol. They also reported sensitivity of 88% and specificity of 96%. In the study mentioned, recognition was correctly conducted for 81% patients [13]. Other study reported Kappa’s correlation coefficient of 0.7 for RUSH [14]. Previous studies have suggested using protocol for better and faster diagnosis [9]. RUSH technique is one of protocols used for early diagnosis and continuous monitoring of patients in emergency departments [11, 15].
There was need to conduct a study for evaluation of accuracy of RUSH in early recognition of emergency department patients. This study was thus conducted to investigate accuracy of RUSH in early recognition of emergency department patients.
Materials and Methods
Patients
A case-control study was conducted in the emergency department of Shahid Mohammadi hospital for detecting accuracy of the RUSH technique. It was approved by the ethics committee of Hormozgan University of Medical Sciences.
Participants
During April 2016 to May 2017, we have recorded all the patients with shock at the emergency department of Shahid Mohammadi hospital and the samples were selected by simple sampling method. On the basis of the time of the patients’ arrival, the emergency physicians or radiologist conducted the sonography exams on the basis of the RUSH procedure concurrent with ongoing care of each patient.
Shock classification and rapid ultrasound in shock protocol
In the current study shock was classified into 4 groups: hypovolemic, cardiogenic, distributive (septic or neurogenic) and obstructive (due to pneumothorax, tamponade, pulmonary thromboembolic disease). Some patients showed a combination of shocks and grouped as mixed type. Some components are used in RUSH exam including evaluation of inferior vena cava, thoracic and abdominal compartments and large arteries and veins. Pericardial effusion, cardiac tamponade, ascite, pleural effusion and pulmonary edema were investigated.
Statistical Analysis
SPSS 20 software was used for analyzing the data. We have evaluated the overall agreement of defined shock types on the basis of RUSH results and final diagnosis of patients via calculating the Kappa index. Subgroup analysis and investigation of Kappa index for results of the RUSH exam were used. The Kappa agreement and reliability indices sensitivity, specificity, positive (PPV) and negative predictive values (NPV) were used.
Findings
Demographic and clinical characteristics
The mean age was 64.04±9.2 (45 to 86) years. Out of 52 patients studied, pulmonary and cardiac signs were as follows; 21 patients with pericardial effusion (40.4%), 9 patients with cardiac tamponade (17.3%), 25 patients with ascite (48.1%), 25 patients with ascite (48.1%), 25 patients with pleural effusion (48.1%) and 18 patients with pulmonary edema (34.6%).
Prevalence of different types of shock
On the basis the procedures, hypovolemic and cardiogenic shocks had most frequent among types of shock (Table 1).
Table 1. Prevalence of hypovolemic (Hyp), cardiogenic (Crd), obstructive (Obs), and distributive (Dis) shock based on final clinical diagnosis and RAUSH exam
The data for accuracy, sensitivity, specificity, PPV, NPV and Kappa index of the protocol for type of shock are shown in Table 2. The results for Kappa index for general agreement between shock types was defined by the RUSH protocol and final diagnosis was 0.85 (p=0.001) for all patients.
Table 2. Reliability indices and Kappa agreement of the rapid ultrasound in shock exam for hypovolemic (Hyp), cardiogenic (Crd), obstructive (Obs), and distributive (Dis) shock
Hypovolemic Shock
The data for hypovolemic shock showed good sensitivity, excellent agreement, specificity and accuracy and highest agreement with final diagnoses were observed for this shock. We had 15 cases finally diagnosed as having hypovolemic shocks who were all observed on the basis of RUSH findings (88.2% sensitivity, and 100% PPV). In the current study, among 17 diagnosed, 15 patients were correctly diagnosed, 1 patient was diagnosed in cardiogenic shock and 1 patient in mixed shock.
Cardiogenic shock
Good sensitivity, excellent specificity, accuracy and agreement were observed for cardiogenic shock. We have correctly distinguished 14 out of 16 cardiogenic shock cases, indicating good sensitivity (87.50%). Other patients were diagnosed as obstructive and mixed respectively. The results showed 87.5%, 97.3%, 94.2%, 93.3%, 97.3% and 0.62 for sensitivity, specificity, accuracy, PPV, NPV and agreement respectively.
Obstructive Shock
The data for obstructive shock showed good sensitivity and agreement, excellent specificity and accuracy. We had 10 cases finally diagnosed as having obstructive shocks in which 9 patients were diagnosed as obstructive on the basis of RUSH findings (96.2% accuracy, and 88.9% PPV). In the current study, other patient was diagnosed as distributive. The results showed 88.9%, 97.7%, 96.2%, 88.9%, 97.7% and 0.77 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively.
Distributive shock
Low agreement, excellent specificity, sensitivity and accuracy were seen in distributive shock. We have found 10 patients with distributive shocks with the early RUSH exam that 9 patients belonged to this shock, showing good sensitivity. The results showed 90.0%, 97.7%, 96.2%, 90.0%, 97.7% and 0.47 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively.
PPV, positive predictive value of RUSH criteria to determine each type of shock; NPV, negative predictive value of RUSH criteria to determine each shock type; Kappa, index of agreement between diagnosis of shock type based on RUSH criteria and final diagnosis.
Discussion
Shock includes conditions that threatens life and is divided into four categories including cardiogenic, hypovolemic, distributive and obstructive [1]. Since different shocks need special treatments, it is needed to use quick-detection techniques for recognition of shock in the emergency department and critical care units [2]. The results showed an acceptable appropriate agreement between the results obtained and final clinical diagnosis of patients (Kappa=0.85). Some fast protocols are increasingly in access for providing associated information to the pathology and management of shocks condition. The RUSH protocol has advantages including learning doing, the simple equipment needed, simplicity and a possible direct vision of volume. A study reported similar agreement for their study that focused on a similar multi-organ sonography assessment of emergency patients [16]. Bagheri Hariri et al. [17] reported Kappa correlation coefficient for comparison of the RUSH technique and the final diagnosis by 0.84% that shows a high compliance rate of the protocol. Another study reported Kappa’s correlation coefficient for comparison of the RUSH by 0.85 [12].
The results show that use of RUSH is appropriate option for early recognition in patients with shock. The RUSH technique is reliable for hypovolemic, cardiogenic or obstructive subtypes (NPV>0.94). These results show that therapeutic approaches used for treatment have appropriate effectiveness, especially for final outcome obtained. Hypovolemic shock is usually occurs due to bleeding or severe fluid loss [12]. The RUSH technique is on the basis of the hyper contractile and small chamber size for diagnosis of hypovolemic shock. The results showed 88.2%, 100%, 96.2%, 100%, 94.6% and 0.98 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively. In summary, the results showed the use of diagnostic RUSH technique in hypovolemic shock management is appropriate. Cardiogenic shock is usually occurs due to pump failure and the inappropriate ability of the heart for moving the needed oxygenated blood toward vital organs. The results showed 87.5%, 97.3%, 94.2%, 93.3%, 97.3% and 0.62 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively. Our findings confirm effectiveness of use of diagnostic RUSH technique in cardiogenic shock management is appropriate. Obstructive shock is most commonly induced through cardiac tamponade, tension pneumothorax, or largepulmonary embolus [12]. The results showed 88.9%, 97.7%, 96.2%, 88.9%, 97.7% and 0.77 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively. Overall, the results confirm effectiveness of use of diagnostic RUSH technique in obstructive shock management is appropriate. Distributive shock is most commonly induced by vascular system vasodilation in point that the core vascular blood volume is insufficient for maintaining organ perfusion [12]. This shock usually occurs following inflammation. Inflammatory response to infection increases by systemic inflammatory response syndrome (SIRS), severe sepsis and septic shock steps. The results showed 90.0%, 97.7%, 96.0%, 90.0%, 97.7% and 0.47 for sensitivity, specificity, accuracy, PPV, NPV and agreement, respectively. In summary, the results showed the use of diagnostic RUSH technique in distributive shock management is appropriate.
Conclusion
In summary, the results obtained for RUSH provided reliable information for clinicians to make a fast and acceptably accurate recognition of the shock type in a hypotensive patient, especially for obstructive, cardiogenic or hypovolemic shock types.
Acknowledgments: None declared by the authors.
Ethical Permission: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
1. Wacker DA, Winters ME. Shock. Emerg Med Clin North Am. 2014;32(4):747-58. [Link] [DOI:10.1016/j.emc.2014.07.003]
2. Wongwaisayawan S, Suwannanon R, Prachanukool T, Sricharoen P, Saksobhavivat N, Kaewlai R. Trauma ultrasound. Ultrasound Med Biol. 2015;41(10): 543-61. [Link] [DOI:10.1016/j.ultrasmedbio.2015.05.009]
3. Volpicelli G, Lamorte A, Tullio M, Cardinale L, Giraudo M, Stefanone V, et al. Point-of-care multiorgan ultrasonography for the evaluation of undifferentiated hypotension in the emergency department. Intensive Care Med. 2013;39(7):1290-8. [Link] [DOI:10.1007/s00134-013-2919-7]
4. Gaieski DF, Mikkelsen M. Definition, classification, etiology, and pathophysiology of shock in adults [Internet]. Tehran: UpToDate. 2017 [Cited 22 June 15]. Available from: https://www.medilib.ir/uptodate/show/1594. [Persian] [Link]
5. Peterson D, Arntfield RT. Critical care ultrasonography. Emerg Med Clin North Am. 2014;32(4):907-26. [Link] [DOI:10.1016/j.emc.2014.07.011]
6. Jones AE, Tayal VS, Sullivan DM, Kline JA. Randomized, controlled trial of immediate versus delayed goal-directed ultrasound to identify the cause of nontraumatic hypotension in emergency department patients. Crit Care Med. 2004;32(8):1703-8. [Link] [DOI:10.1097/01.CCM.0000133017.34137.82]
7. Atkinson PRT, McAuley DJ, Kendall RJ. Abdominal and cardiac evaluation with sonography in shock (ACES): An approach by emergency physicians for the use of ultrasound in patients with undifferentiated hypotension. Emergency Med J. 2009;26(2):87-91. [Link] [DOI:10.1136/emj.2007.056242]
8. Gunst M, Ghaemmaghami V, Sperry J. Accuracy of cardiac function and volume status estimates using the bedside echocardiographic assessment in trauma/critical care. The J Trauma. 2008;65(3):509-16. [Link] [DOI:10.1097/TA.0b013e3181825bc5]
9. Perera P, Mailhot T, Riley D, Mandavia D. The RUSH exam: Rapidultrasound in shock in the evaluation of critically ill patient. Emerg MedClin North Am. 2010;28(1):29-56. [Link] [DOI:10.1016/j.emc.2009.09.010]
10. Perera P, Mailhot T, Riley D, Mandavia D. The RUSH Exam 2012: Rapidultrasound in shock in the evaluation of critically ill patient. Ultrasound Clin. 2012;7:255-78. [Link] [DOI:10.1016/j.cult.2011.12.010]
11. Seif D, Perera P, Mailhot T, Riley D, Mandavia D. Bedside ultrasound in resuscitation and the rapid ultrasound in shock protocol. Crit Care Res Pract. 2012;2012:503254. [Link] [DOI:10.1155/2012/503254]
12. Keikha M, Salehi-Marzijarani M, SoldooziNejat R, Sheikh MotaharVahedi H, Mirrezaie SM. Diagnostic Accuracy of Rapid Ultrasound in Shock (RUSH) Exam; A systematic review and meta-analysis. Bull Emerg Trauma. 2018;6(4):271-8. [Link] [DOI:10.29252/beat-060402]
13. Deville WL, Buntinx F, Bouter LM, Montori VM, de Vet HC, van der Windt DA, et al. Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol. 2002;2:9. [Link] [DOI:10.1186/1471-2288-2-9]
14. Jones CM, Athanasiou T. Summary receiver operating characteristic curve analysis techniques in the evaluation of diagnostic tests. Ann Thorac Surg. 2005;79(1):16-20. [Link] [DOI:10.1016/j.athoracsur.2004.09.040]
15. Hernandez C, Shuler K, Hannan H, Sonyika C, Likourezos A, Mar¬shall J. C.A.U.S.E.: Cardiac arrest ultra-sound exam-a better approach to managing patients in primary non-arrhythmogenic cardiac arrest. Resuscitation. 2008;76(2):198-206. [Link] [DOI:10.1016/j.resuscitation.2007.06.033]
16. Dwamena B. MIDAS: Stata module for meta-analytical integration of diagnostic test accuracy studies. Statistical Software Components. 2009;10:23-32. [Link]
17. Bagheri-Hariri S, Yekesadat M, Farahmand S, Arbab M, Sedaghat M, Shahlafar N, et al. The impact of using RUSH protocol for diagnosing the type of unknown shock in the emergency department. Emerg Radiol. 2015;22(5):517-20. [Link] [DOI:10.1007/s10140-015-1311-z]