GMJ Medicine
eISSN : 2626-3041
Volume 4, Issue 1 (2025)
GMJM 2025, 4(1): 31-35 |
Back to browse issues page
History
Received: 2024/07/8 | Accepted: 2024/11/25 | Published: 2025/01/14
Received: 2024/07/8 | Accepted: 2024/11/25 | Published: 2025/01/14
How to cite this article
Dzigandzli G, Askaripour M, Rajabi S, Shahmoradi M. Effects of Curcumin on GLUT4, Erα and Insulin Resistance Genes Expression in Polycystic Ovary Syndrome Rats. GMJM 2025; 4 (1) :31-35
URL: http://gmedicine.de/article-2-247-en.html
URL: http://gmedicine.de/article-2-247-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Georgian Center for Neuroscience Research, International Center for Intelligent Research, Tbilisi, Georgia
2- Department of Physiology, School of Medicine, Bam University of Medical Sciences, Bam, Iran
3- Department of General Surgery, Lorestan University of Medical Sciences, Khorramabad, Iran
2- Department of Physiology, School of Medicine, Bam University of Medical Sciences, Bam, Iran
3- Department of General Surgery, Lorestan University of Medical Sciences, Khorramabad, Iran
Keywords:
| Abstract (HTML) (2763 Views)
Full-Text: (835 Views)
Introduction
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders that induces anovulation in the women and animals [1].
Some metabolic abnormalities including dyslipidemia, insulin resistance, diabetes, obesity, and infertility occur in patients with PCOS [2, 3]. PCOS has been known with some signs including production of small arrested antral follicle, decreased estrogen and increased LH/FSH ratio [4].
Insulin signaling pathway could have major role in pathogenesis of PCOS which comprises pathways of phosphatidylinositol 3 kinase (PI3K) and protein kinase B/Akt signaling [5-7].
Selective insulin resistance can progress and in such cases, metabolic response to insulin action has been faulted including PI3K pathway, however, other actions are not only maintained but may be increased, including the mitogen activated protein kinase (MAPK) pathway, in insulin group target tissues and ovary [5, 6]. Insulin joins to its receptor and acts insulin receptor substrate (IRS) through the phosphorylation of tyrosine residues. The expression of IRS in the uterus has been reported [7] and glucose metabolism is essential for uterine cell differentiation [8].
It has been known that GLUT4 is the most important glucose transporter isoform in insulin-dependent tissues and modulates ininsulin-stimulated glucose transport in the uterus [9]. Different studies have reported decreased GLUT4 expression in the uterus of PCOS patients [10, 11].
Oestrogen receptor α (ERα) has been known to have an essential role [12], for example ER-knockout rats are infertile [13-15]. Some common hormonal therapies are used to treat the PCOS condition and to stimulate the ovulation. These treatments cause adverse effects on arthritis, joint or muscle pain [16] and psychological disturbances [17]. There is a great attention on medicines from natural sources that are safe and useful. Curcumin, is a natural active in turmeric, has biological effects including anti-inflammatory, antioxidant [18], hypoglycaemic [19] and anti-hyperlipidemic activities. It is known to have anti-proliferative and apoptotic activities in some human cancer cell lines, such as cells obtained from cancers of prostate, breast and ovary [20-22].
It seems that curcumin could improve the gene expression of GLUT4 and ERα and other related parameters in rats with PCOS. Therefore, this study was conducted to evaluate the effects of curcumin on insulin resistance (IR) and uterine gene expression of GLUT4 and ERα in rats with PCOS.
Materials and Methods
Animals
Sixty Sprague–Dawley female rats with weight of 180±5g were used for this study. All the animals were grouped in a 25°C a lighting diet 12:12 h light:dark cycle. The animals had ad libitum access to conventional feed pellets and water. To evaluate the body weight changes, we have weighed animals in start and end of the trial.
All animals were randomly grouped into 4 groups (n=15):
1) Control group without PCOS (Positive Control);
2) PCOS group without treatment (Negative Control);
3) PCOS rats treated with daily oral doses of 100mg/kg daily (Cur-100); and
4) PCOS rats treated with daily oral doses of 200mg/kg daily (Cur-200).
Curcumin (Sigma; USA) was dissolved in 0.5% carboxy methyl cellulose per oral for 30 days. To induce the PCOS, animals were subcutaneously administrated with 6 mg dehydroepiandrosterone (DHEA) per 100g day-1(DHEA dissolved in 0.2 mL sesame oil) for 21 consecutive days [23]. Following administration of curcumin (after 30 days), 5 animals per group were killed and some tissues including ovaries and uterus were collected and blood samples were collected to prepare the serum.
Evaluation of IR
The blood samples were used to evaluate the fasting blood glucose (FBG) and fasting insulin serum (FIS) levels. FBG was assessed by glucose oxidase procedure and FIS was assessed by a direct competitive enzyme-linked immunosorbent assay (ELISA) kit [24]. The optical values were read in the 450nm by a microplate reader and the induction of IR was investigatedby the homeostasis model assessment of insulin resistance (HOMA-IR) method. HOMA-IR was calculated using the following formula:
HOMA-IR = FBG (mmol/L) × FIS (mU/L) / 22.50
Rat ovarian morphology
All the animals’ ovaries were prepared by surgery fixed in 10% formalin and included in paraffin. Sections prepared were stained by haematoxylin and eosin then evaluated by two pathologists that did not information from the sample type for ovarian morphological properties.
Gene expression of GLUT4 and Erα
Endometrium RNA isolation and real-time polymerase chain reaction (PCR) were conducted as reported by others [25]. The primers sequences were GLUT4, forward (5'- GGGCTGTGAGTGAGTGCTTTC-3') and reverse (5'- CAGCGAGGCAAGGCTAGA-3'); Erα, forward (5'-CCAAAGCCTCGGGAATGG-3') and reverse (5'- AGCTGCGGGCGATTGAG-3'); and β-actin, forward (5'- AAGGCCAACCGTGAAAAGAT-3') and reverse (5'-ACCAGAGGCATACAGGGAC-3').
Statistical analysis
SPSS 21 software was used to analysis the data by tukey test (difference between groups). The level of statistical significance was set at p<0.05.
Findings
Body weight
Effects of experimental treatments on body weight of rats with PCOS are shown in Figure 1. As results show, body weight was significantly higher in rats with PCOS in comparison to those in control group (p<0.05). Oral administration of curcumin in the both levels (100 and 200mg) significantly decreased adverse effects of PCOS on body weight and better response was observed in higher dose (p<0.05).
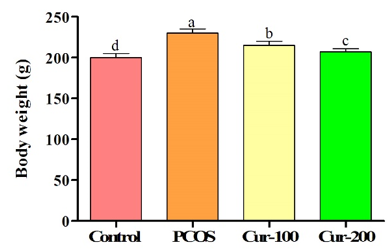
Figure 1. Effects of oral administration of curcumin on body weight (g) of rats with PCOS. Superscripts (a-d) show significant difference between groups.
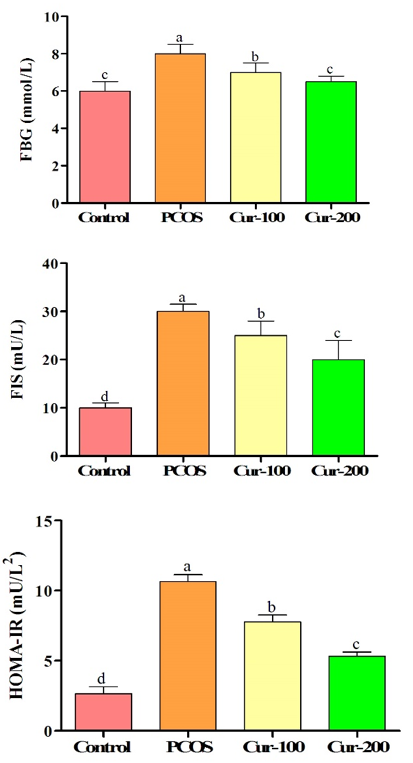
Figure 2. Effects of oral administration of curcumin on insulin resistance of rats with PCOS. Superscripts (a-d) show significant difference between groups.
Insulin resistance
PCOS increased levels of FIS, FBG and HOMA-IR in comparison to control group (p<0.05). Oral administration of curcumin could significantly decrease levels of FIS, FBG and HOMA-IR (p<0.05; Figure 2).
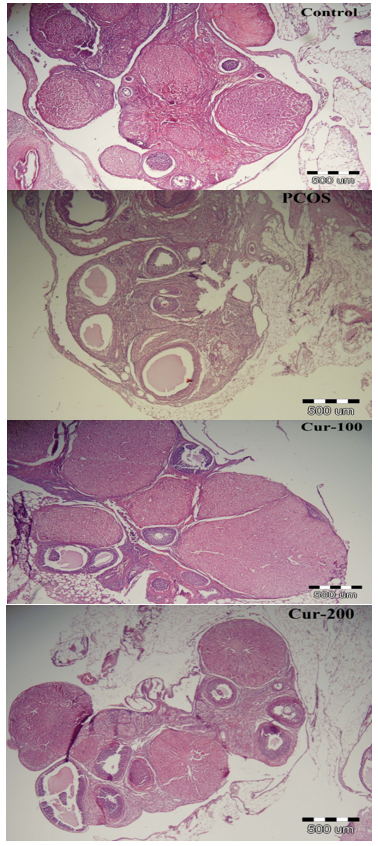
Figure 3. Effects of oral administration of curcumin on ovarian morphology of rats with PCOS
Ovarian morphology
In the control group, the follicles were normal, but ovaries of rats in the PCOS group had an increase in ovarian volume, decreased corpus luteum and theca layer hypertrophy and thickening in comparison to control group. Cystic follicles were also observed in PCOS group that means induction of PCOS. Oral administration of curcumin alleviated cystic follicles and increased corpus luteum (Figure 3).
Gene expression
Effects of oral administration of curcumin on gene expression of GLUT4 and Erα of rats with PCOS are shown in Figure 4. Induction of PCOS decreased expression of GLUT4 and Erα (p<0.05). The use of higher levels of curcumin increased expression of GLUT4 and Erα (p<0.05). The use of lower level could also increase GLUT4 and Erα expression (p<0.05; Figure 4).
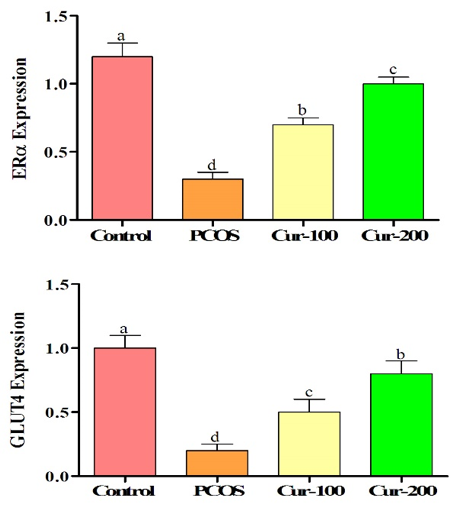
Figure 4. Effects of oral administration of curcumin on gene expression of GLUT4 and Erα of rats with PCOS. Superscripts (a-d) show significant difference between groups.
Discussion
PCOS is one of the disorder related with diabetes and causes with signs such as hyperglycemia in first stages that gradually induces IR [26]. In the current study, rats induced with PCOS indicated an increase in FIS, FBG and HOMA-IR. Hyperglycaemia is result from IR, but the exact mechanism of PCOS is still not known. Previous studies have shown faulted insulin intracellular signaling, particularly alterations in insulin receptor substance-1 (IRS-1) phosphorylation that may be a factor for PCOS-IR [27]. On the other hand, adipose tissue increases the release of pro-inflammatory cytokines [28] and changesIRS-1 tyrosine phosphorylation to serine phosphorylation, which initiates IR. Our findings also showed that the body weight was significantly higher in PCOS rats. It seems overweight promotes to produce pro-inflammatory cytokines and promotes IR. Oral administration of curcumin improved IR, especially in higher doses. Improved IR could be attributed to anti-inflammatory properties of curcumin that prevents production of pro-inflammatory cytokines [18]. On the other hand, curcumin decreased body weight that in turn decreases IR. As results showed, oral administration of curcumin decreased levels of FBG and FIS. Decreased levels of FBG could be attributed to increased expression of GLUT4 in rats treated with curcumin. Transformation on cell surface by GLUT4 relies on insulin signaling pathway [29] and IR decreases GLUT4 expression [30]. Not only GLUT4 but also ERα are involved in glucose metabolism. Increased ERα expression promotes the sensitivity of skeletal muscle cells to insulin and causes to consume the glucose [31]. It is clear that curcumin improves IR through involvement in the expression of GLUT4 andERα. Another study showed that curcumin increases the gene expression of GLUT4 but synergistic effects of curcumin and insulin is stronger in comparison to insulin that could be attributed to the competitive activity of insulin and curcumin in activation of gene expression [32]. It could be speculated that curcumin could improve insulin resistance by influencing on GLUT4 and ERα gene expression. Rats with PCOS showed a number of cystic follicles and decreased corpus luteum. Similar results were reported by previous studies [25]. Oral administration of curcumin could decrease cystic follicles and increase corpus luteum. Increased corpora lutea implicates ovulation and normal estrous cyclicity.
Follicles in the different steps of development with oocytes and clear, visible granulosa cell layer were seen in curcumin groups.
Conclusion
Curcumin has a protective effect in patients with PCOS and oral administration of curcumin prevents diabetes. Curcumin usage decrease the insulin resistance and increase expression of GLUT4 and Erα.
Acknowledgements: None declared by the authors.
Ethical Permission: Compliance with ethical guidelines, approval for this study was obtained from International Center for Intelligent Research.
Conflicts of Interests: None declared by the authors.
Authors' Contribution: All authors contributed toward data analysis, drafting and revising the paper and agreed to be responsible for all the aspects of this work.
Funding/Support: This study was supported by a grant from International Center for Intelligent Research (ICIR-2018-184157).
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders that induces anovulation in the women and animals [1].
Some metabolic abnormalities including dyslipidemia, insulin resistance, diabetes, obesity, and infertility occur in patients with PCOS [2, 3]. PCOS has been known with some signs including production of small arrested antral follicle, decreased estrogen and increased LH/FSH ratio [4].
Insulin signaling pathway could have major role in pathogenesis of PCOS which comprises pathways of phosphatidylinositol 3 kinase (PI3K) and protein kinase B/Akt signaling [5-7].
Selective insulin resistance can progress and in such cases, metabolic response to insulin action has been faulted including PI3K pathway, however, other actions are not only maintained but may be increased, including the mitogen activated protein kinase (MAPK) pathway, in insulin group target tissues and ovary [5, 6]. Insulin joins to its receptor and acts insulin receptor substrate (IRS) through the phosphorylation of tyrosine residues. The expression of IRS in the uterus has been reported [7] and glucose metabolism is essential for uterine cell differentiation [8].
It has been known that GLUT4 is the most important glucose transporter isoform in insulin-dependent tissues and modulates ininsulin-stimulated glucose transport in the uterus [9]. Different studies have reported decreased GLUT4 expression in the uterus of PCOS patients [10, 11].
Oestrogen receptor α (ERα) has been known to have an essential role [12], for example ER-knockout rats are infertile [13-15]. Some common hormonal therapies are used to treat the PCOS condition and to stimulate the ovulation. These treatments cause adverse effects on arthritis, joint or muscle pain [16] and psychological disturbances [17]. There is a great attention on medicines from natural sources that are safe and useful. Curcumin, is a natural active in turmeric, has biological effects including anti-inflammatory, antioxidant [18], hypoglycaemic [19] and anti-hyperlipidemic activities. It is known to have anti-proliferative and apoptotic activities in some human cancer cell lines, such as cells obtained from cancers of prostate, breast and ovary [20-22].
It seems that curcumin could improve the gene expression of GLUT4 and ERα and other related parameters in rats with PCOS. Therefore, this study was conducted to evaluate the effects of curcumin on insulin resistance (IR) and uterine gene expression of GLUT4 and ERα in rats with PCOS.
Materials and Methods
Animals
Sixty Sprague–Dawley female rats with weight of 180±5g were used for this study. All the animals were grouped in a 25°C a lighting diet 12:12 h light:dark cycle. The animals had ad libitum access to conventional feed pellets and water. To evaluate the body weight changes, we have weighed animals in start and end of the trial.
All animals were randomly grouped into 4 groups (n=15):
1) Control group without PCOS (Positive Control);
2) PCOS group without treatment (Negative Control);
3) PCOS rats treated with daily oral doses of 100mg/kg daily (Cur-100); and
4) PCOS rats treated with daily oral doses of 200mg/kg daily (Cur-200).
Curcumin (Sigma; USA) was dissolved in 0.5% carboxy methyl cellulose per oral for 30 days. To induce the PCOS, animals were subcutaneously administrated with 6 mg dehydroepiandrosterone (DHEA) per 100g day-1(DHEA dissolved in 0.2 mL sesame oil) for 21 consecutive days [23]. Following administration of curcumin (after 30 days), 5 animals per group were killed and some tissues including ovaries and uterus were collected and blood samples were collected to prepare the serum.
Evaluation of IR
The blood samples were used to evaluate the fasting blood glucose (FBG) and fasting insulin serum (FIS) levels. FBG was assessed by glucose oxidase procedure and FIS was assessed by a direct competitive enzyme-linked immunosorbent assay (ELISA) kit [24]. The optical values were read in the 450nm by a microplate reader and the induction of IR was investigatedby the homeostasis model assessment of insulin resistance (HOMA-IR) method. HOMA-IR was calculated using the following formula:
HOMA-IR = FBG (mmol/L) × FIS (mU/L) / 22.50
Rat ovarian morphology
All the animals’ ovaries were prepared by surgery fixed in 10% formalin and included in paraffin. Sections prepared were stained by haematoxylin and eosin then evaluated by two pathologists that did not information from the sample type for ovarian morphological properties.
Gene expression of GLUT4 and Erα
Endometrium RNA isolation and real-time polymerase chain reaction (PCR) were conducted as reported by others [25]. The primers sequences were GLUT4, forward (5'- GGGCTGTGAGTGAGTGCTTTC-3') and reverse (5'- CAGCGAGGCAAGGCTAGA-3'); Erα, forward (5'-CCAAAGCCTCGGGAATGG-3') and reverse (5'- AGCTGCGGGCGATTGAG-3'); and β-actin, forward (5'- AAGGCCAACCGTGAAAAGAT-3') and reverse (5'-ACCAGAGGCATACAGGGAC-3').
Statistical analysis
SPSS 21 software was used to analysis the data by tukey test (difference between groups). The level of statistical significance was set at p<0.05.
Findings
Body weight
Effects of experimental treatments on body weight of rats with PCOS are shown in Figure 1. As results show, body weight was significantly higher in rats with PCOS in comparison to those in control group (p<0.05). Oral administration of curcumin in the both levels (100 and 200mg) significantly decreased adverse effects of PCOS on body weight and better response was observed in higher dose (p<0.05).
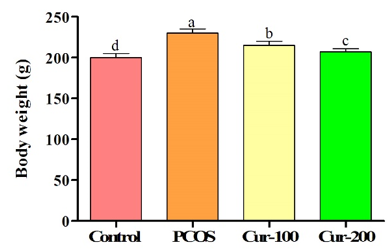
Figure 1. Effects of oral administration of curcumin on body weight (g) of rats with PCOS. Superscripts (a-d) show significant difference between groups.
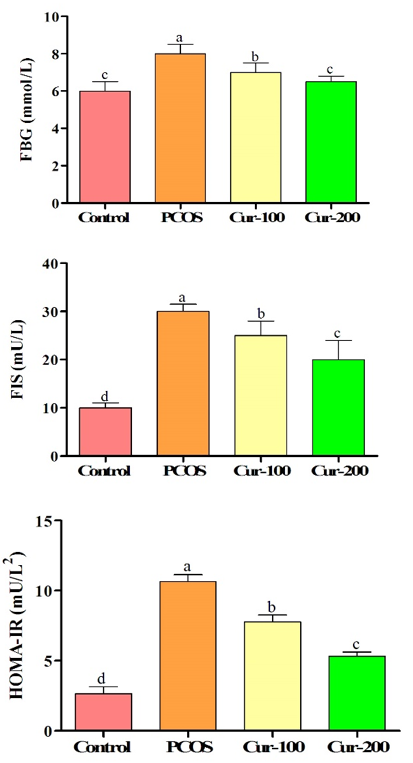
Figure 2. Effects of oral administration of curcumin on insulin resistance of rats with PCOS. Superscripts (a-d) show significant difference between groups.
Insulin resistance
PCOS increased levels of FIS, FBG and HOMA-IR in comparison to control group (p<0.05). Oral administration of curcumin could significantly decrease levels of FIS, FBG and HOMA-IR (p<0.05; Figure 2).
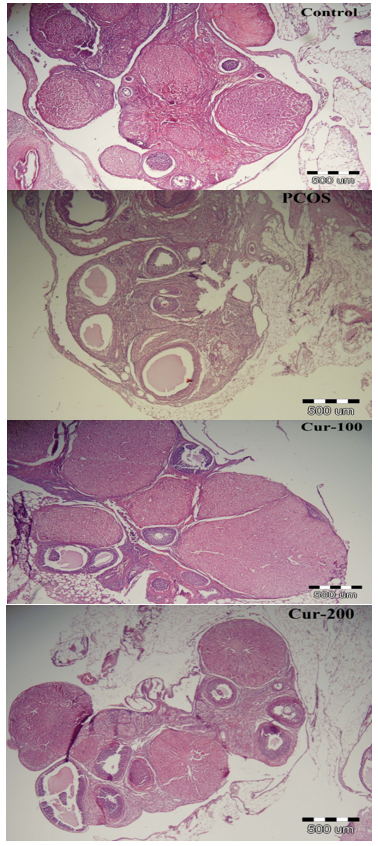
Figure 3. Effects of oral administration of curcumin on ovarian morphology of rats with PCOS
Ovarian morphology
In the control group, the follicles were normal, but ovaries of rats in the PCOS group had an increase in ovarian volume, decreased corpus luteum and theca layer hypertrophy and thickening in comparison to control group. Cystic follicles were also observed in PCOS group that means induction of PCOS. Oral administration of curcumin alleviated cystic follicles and increased corpus luteum (Figure 3).
Gene expression
Effects of oral administration of curcumin on gene expression of GLUT4 and Erα of rats with PCOS are shown in Figure 4. Induction of PCOS decreased expression of GLUT4 and Erα (p<0.05). The use of higher levels of curcumin increased expression of GLUT4 and Erα (p<0.05). The use of lower level could also increase GLUT4 and Erα expression (p<0.05; Figure 4).
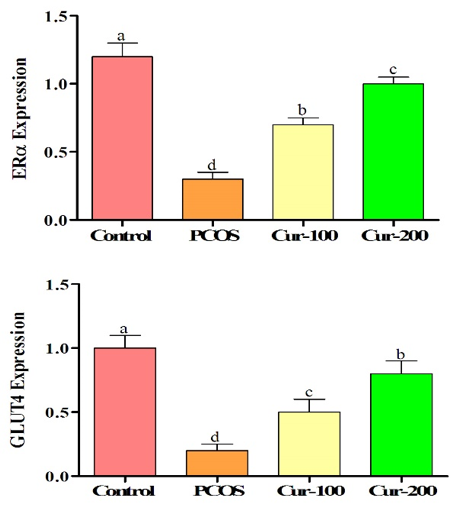
Figure 4. Effects of oral administration of curcumin on gene expression of GLUT4 and Erα of rats with PCOS. Superscripts (a-d) show significant difference between groups.
Discussion
PCOS is one of the disorder related with diabetes and causes with signs such as hyperglycemia in first stages that gradually induces IR [26]. In the current study, rats induced with PCOS indicated an increase in FIS, FBG and HOMA-IR. Hyperglycaemia is result from IR, but the exact mechanism of PCOS is still not known. Previous studies have shown faulted insulin intracellular signaling, particularly alterations in insulin receptor substance-1 (IRS-1) phosphorylation that may be a factor for PCOS-IR [27]. On the other hand, adipose tissue increases the release of pro-inflammatory cytokines [28] and changesIRS-1 tyrosine phosphorylation to serine phosphorylation, which initiates IR. Our findings also showed that the body weight was significantly higher in PCOS rats. It seems overweight promotes to produce pro-inflammatory cytokines and promotes IR. Oral administration of curcumin improved IR, especially in higher doses. Improved IR could be attributed to anti-inflammatory properties of curcumin that prevents production of pro-inflammatory cytokines [18]. On the other hand, curcumin decreased body weight that in turn decreases IR. As results showed, oral administration of curcumin decreased levels of FBG and FIS. Decreased levels of FBG could be attributed to increased expression of GLUT4 in rats treated with curcumin. Transformation on cell surface by GLUT4 relies on insulin signaling pathway [29] and IR decreases GLUT4 expression [30]. Not only GLUT4 but also ERα are involved in glucose metabolism. Increased ERα expression promotes the sensitivity of skeletal muscle cells to insulin and causes to consume the glucose [31]. It is clear that curcumin improves IR through involvement in the expression of GLUT4 andERα. Another study showed that curcumin increases the gene expression of GLUT4 but synergistic effects of curcumin and insulin is stronger in comparison to insulin that could be attributed to the competitive activity of insulin and curcumin in activation of gene expression [32]. It could be speculated that curcumin could improve insulin resistance by influencing on GLUT4 and ERα gene expression. Rats with PCOS showed a number of cystic follicles and decreased corpus luteum. Similar results were reported by previous studies [25]. Oral administration of curcumin could decrease cystic follicles and increase corpus luteum. Increased corpora lutea implicates ovulation and normal estrous cyclicity.
Follicles in the different steps of development with oocytes and clear, visible granulosa cell layer were seen in curcumin groups.
Conclusion
Curcumin has a protective effect in patients with PCOS and oral administration of curcumin prevents diabetes. Curcumin usage decrease the insulin resistance and increase expression of GLUT4 and Erα.
Acknowledgements: None declared by the authors.
Ethical Permission: Compliance with ethical guidelines, approval for this study was obtained from International Center for Intelligent Research.
Conflicts of Interests: None declared by the authors.
Authors' Contribution: All authors contributed toward data analysis, drafting and revising the paper and agreed to be responsible for all the aspects of this work.
Funding/Support: This study was supported by a grant from International Center for Intelligent Research (ICIR-2018-184157).
References
1. Arikawe AP, Iranloye BO, Ogunsola AO, Daramola AO. Chronic fructose consumption as a model of polycystic ovary syndrome in pregnant female sprague- dawley rats. Afr J Biomed Res. 2013;15(1):7-13. [Link]
2. Zhai HL, Wu H, Xu H, Weng P, Xia FZ, Chen Y, Lu YL. Trace glucose andlipid metabolism in high androgen and high-fat diet induced polycystic ovarysyndrome rats. Reprod Biol Endocrinol. 2012;10:5. [Link] [DOI:10.1186/1477-7827-10-5]
3. Ghasemzadeh A, Farzadi L, Khaki A, Ahmadi SK. Effect of Allium cepa seeds ethanolic extract on experimental polycystic ovary syndrome (PCOS) apoptosis induced by estradiol-valerate. Life Sci J. 2013;10:170-5. [Linkv]
4. Demirel MA, Ilhan M, Suntar I, Keles H, Akkol EK. Activity ofCorylusavellana seed oil in letrozole-induced polycystic ovary syndrome model in rats. Rev Bras de Farmacogn. 2016;26(1):83-8. [Link] [DOI:10.1016/j.bjp.2015.09.009]
5. Makker A, Goel MM, Das V, Agarwal A. PI3K Akt mTOR and MAPK signaling pathways in polycystic ovarian syndrome, uterine leiomyomas and endometriosis: An update. Gynecol Endocrinol. 2012;28(3):175-81 [Link] [DOI:10.3109/09513590.2011.583955]
6. Zhao Y, Zhang C, Huang Y, Yu Y, Li R, Li M, et al. Up regulated expression of WNT5a increases inflammation and oxidative stress via PI3K/AKT/NF κB signaling in the granulosa cells of PCOS patients. J Clin Endocrinol Metab. 2015;100(1):201-11. [Link] [DOI:10.1210/jc.2014-2419]
7. Skrgatić L, Baldani DP, Gersak K, Cerne JZ, Ferk P and Corić M. Genetic polymorphisms of INS, INSR and IRS 1 genes are not associated with polycystic ovary syndrome in Croatian women. Coll Antropol. 2013;37:141-6. [Link]
8. Strowitzki T, von Eye HC,Kellerer M, Haring HU. Tyrosine kinase activity of insulin-like growth factor I and insulin receptors in human endometrium during the menstrual cycle: Cyclic variation of insulin receptor expression. Fertil Steril. 1993;59(2):315-22. [Link] [DOI:10.1016/S0015-0282(16)55674-X]
9. Sheets EE, Tsibris JC, Cook NI, Virgin SD, DeMay RM, Spellacy WN. In vitro binding of insulin and epidermal growth factor to human endometrium and endocervix. Am J Obstet Gynecol. 1985;153(1):60-5. [Link] [DOI:10.1016/0002-9378(85)90591-5]
10. Mioni R, Chiarelli S, Xamin N, Zuliani L, Granzotto M, MozzanegaB, et al. Evidence for the presence of glucose transporter 4 in the endometriumand its regulation in polycystic ovary syndrome patients. J Clin Endocrinol Metab. 2004;89(8):4089-96. [Link] [DOI:10.1210/jc.2003-032028]
11. Zhai J, Liu CX, Tian ZR, Jiang QH, Sun YP. Effects ofmetformin on the expression ofGLUT4in endometrium of obese womenwith polycystic ovary syndrome. Biol Reprod. 2012;87(2):29. [Link] [DOI:10.1095/biolreprod.112.099788]
12. Carvajal R, Rosas C, Kohan K, Gabler F, Vantman D, Romero C, et al. Metformin augments the levels of molecules that regulate the expression of the insulin- dependent glucose transporter GLUT4 in the endometria of hyperinsulinemic PCOS patients. Hum Reprod. 2013;28(8):2235-44. [Link] [DOI:10.1093/humrep/det116]
13. Hulchiy M, Nybacka A, Sahlin L, Hirschberg AL. Endometrial expression of estrogen receptors and the androgen receptor in women with polycystic ovary syndrome: a lifestyle intervention study. J Clin Endocrinol Metab. 2016;101(2):561-71. [Link] [DOI:10.1210/jc.2015-3803]
14. Meyer MR, Clegg DJ, Prossnitz ER, Barton M. Obesity,insulin resistance and diabetes: Sex differences and role of oestrogen receptors. Acta Physiol (Oxf). 2011;203(1), 259-69. [Link] [DOI:10.1111/j.1748-1716.2010.02237.x]
15. Quaynor SD, Stradtman EW, Kim HG, Shen Y, Chorich LP, Schreihofer DA, et al. Delayed puberty and estrogen resistance in a woman with estrogen receptor alpha variant. N Engl J Med. 2013;369(2):164-71. [Link] [DOI:10.1056/NEJMoa1303611]
16. Badawy A, Elnashar A. Treatment options for polycystic ovary syndrome. Int J Womens Health. 2011;3:25-35. [Link] [DOI:10.2147/IJWH.S11304]
17. Choi SH, Shapiro H, Robinson GE, Irvine J, Neuman J, Rosen B, et al. Psychological side-effects of clomiphene citrate and human menopausal gonadotrophin. J Psychosom Obstet Gynaecol. 2005;26(2):93-100. [Link] [DOI:10.1080/01443610400022983]
18. Pari L, Murugan P. Effect of tetrahydrocurcumin on blood glucose, plasma insulin and hepatic key enzymes in streptozotocin induced diabetic rats. J Basic Clin Physiol Pharmacol. 2005;16(4):257-74. [Link] [DOI:10.1515/JBCPP.2005.16.4.257]
19. Pari L, Murugan P. Antihyperlipidemic effect of curcumin andtetrahydrocurcumin in experimental type 2 diabetic rats. Ren Fail. 2007;29(7):881-9. [Link] [DOI:10.1080/08860220701540326]
20. Aggarwal BB, Banerjee S, Bharadwaj U, Sung B, Shishodia S, Sethi G. Curcumin induces the degradation of cyclin E expression through ubiquitin-dependent pathway and up-regulates cyclindependent kinase inhibitors p21 and p27 in multiple human tumorcell lines. Biochem Pharmacol. 2007;73(7): 1024-32. [Link] [DOI:10.1016/j.bcp.2006.12.010]
21. Watson JL, Greenshields A, Hill R, Hilchie A, Lee PW, Giacomantonio CA, et al. Curcumin-induced apoptosis in ovarian carcinoma cells is p53-independent and involves p38 mitogen-activated protein kinase activation and downregulation of Bcl-2 and survivin expression and Akt signaling. Mol Carcinog. 2010;49(1):13-24. [Link] [DOI:10.1002/mc.20571]
22. Kadasi At, Sirotkin AV, Maruniakova N, Kolesarova A, Bulla J, Grossmann R. The effect ofCurcumin on secretory activity, proliferation and apoptosis of theporcine ovarian granulose cells. J Microbiol Biotechnol Food Sci. 2012;2(1):349-57. [Link]
23. Kavitha A, Narendra B, Sathish K, Veena K. Evaluation of effects of Commiphora Wightii in dehydroepiandrosterone (DHEA) induced polycystic ovary syndrome (PCOS) in rats. PharmaTutor.2016;4(1):47-55. [Link]
24. Miladpour B, Rasti M, Owji AA, Mostafavipour Z, Khoshdel Z, Noorafshan A, et al. Quercetin potentiates transdifferentiation of bone marrow mesenchymal stem cells into the beta cells in vitro. J Endocrinol Invest. 2017;40(5):513-21. [Link] [DOI:10.1007/s40618-016-0592-8]
25. Neisy A, Zal F, Seghatoleslam A, Alaee S. Amelioration by quercetin of insulin resistance and uterine GLUT4 and ERa gene expression in rats with polycystic ovary syndrome (PCOS). 2018;31(2):315-23. [Link] [DOI:10.1071/RD18222]
26. Mesbahzadeh B, Garmsiri M, Jalalvand F, Shojaie L, Kakar MA. Oral administration of menthol could alleviate adverse effects of polycystic ovarian syndrome in blood biochemical parameters and antioxidant status in experimental Wister rats. GMJ Med. 2017;1(1):9-14. [Persian] [Link] [DOI:10.29088/GMJM.2017.09]
27. Diamanti Kandarakis E, Argyrakopoulou G, Economou F, Kandaraki E, Koutsilieris M. Defects in insulin signaling pathways in ovarian steroidogenesis and other tissues in polycystic ovary syndrome (PCOS). J Steroid Biochem Mol Biol. 2008;109(3-5):242-6. [Link] [DOI:10.1016/j.jsbmb.2008.03.014]
28. Winkler G, Kiss S, Keszthelyi L, Sa'pi Z, Ory I, Salamon F, et al. Expression of tumor necrosis factor (TNF)-alpha protein in the subcutaneous and visceral adipose tissue in correlation with adipocyte cell volume, serum TNF-alpha, soluble serum TNF-receptor-2 concentrations and C-peptide level. Eur J Endocrinol. 2003;149(2):129-35. [Link] [DOI:10.1530/eje.0.1490129]
29. Patel N, Huang C, Klip A. Cellular location of insulin-triggered signals and implications for glucose uptake. Pflugers Arch. 2006;451(4):499-510. [Link] [DOI:10.1007/s00424-005-1475-6]
30. Fornes R, Ormazabal P, Rosas C, Gabler F, Vantman D, Romero C, et al. Changes in the expression of insulin signaling pathway molecules in endometria from polycystic ovary syndrome women with or without hyperinsulinemia. Mol Med. 2010;16(3-4):129-36. [Link] [DOI:10.2119/molmed.2009.00118]
31. Riant E, Waget A, Cogo H, Arnal JF, Burcelin R, Gourdy P. Estrogens protect against high-fat diet-induced insulin resistance and glucose intolerance in mice. Endocrinology. 2009;150(5):2109-17. [Link] [DOI:10.1210/en.2008-0971]
32. Moradi A, Bahrami M, Eslami G, Mohiti Ardekani J. The Effect of Curcumin on GLUT4 gene expression as a diabetic resistance marker in C2C12 myoblast cells. Iran J Diabetes Obesity.2014;6(2):98-105. [Link]









