GMJ Medicine
eISSN : 2626-3041
Volume 2, Issue 3 (2023)
GMJM 2023, 2(3): 77-80 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2023/01/25 | Accepted: 2023/06/29 | Published: 2023/08/15
Received: 2023/01/25 | Accepted: 2023/06/29 | Published: 2023/08/15
How to cite this article
Mahdavi F, Azhough R. Effectiveness of Metronidazole Ointment on the Pain of Hemorrhoidectomy Patients. GMJM 2023; 2 (3) :77-80
URL: http://gmedicine.de/article-2-201-en.html
URL: http://gmedicine.de/article-2-201-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
F. Mahdavi1, R. Azhough *1
1- Tuberculosis and Lung Disease Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Keywords:
| Abstract (HTML) (3811 Views)
Full-Text: (2511 Views)
Introduction
Hemorrhoid is one of the most common diseases of the gastrointestinal tract, which causes pain and bleeding due to local damage to the black veins in the anal area during defecation [1].
If this disorder is not controlled and treated on an outpatient basis, surgery is one of the good methods in treating hemorrhoids. But hemorrhoidectomy can also cause complications such as pain, bleeding, urinary retention, infection, compression and thickening of the stool, and damage to the internal sphincter [2]. In the meantime, it seems that several factors are involved in the occurrence of pain after hemorrhoidectomy, such as patient tolerance, type B anesthesia, postoperative analgesia, as well as surgical techniques [3, 4].
Therefore, in order for the patient to be able to tolerate this type of treatment, reducing the pain after hemorrhoids has always been an important goal [5]. Numerous studies have been performed to reduce pain after hemorrhoid surgery, including the use of 0.2% nitroglycerin ointment, which is helpful in relaxing the anal sphincter in the initial pain after hemorrhoidectomy, but the complication of headache following the use of this product appears sometimes unbearable for the patient and limits the use of this product [6].
Inhibition of the posterior areas around the anus by rupivacaine 0.75% to control pain, although it leads to an immediate analgesic effect, pain relief after surgery does not last long and is sometimes associated with serious problems [7, 8].
The use of fentanyl percutaneously and a subcutaneous morphine injection pump, despite effective pain control, can be costly and addictive. The use of botulinum toxin after hematoid hemorrhoids, although significantly reduces pain, due to the high cost of treatment and its injection by skilled professionals, it is not possible to use it for the general public [9, 10].
Recently, the use of metronidazole in reducing pain after hemorrhoids has been considered and it has been shown that the oral form of this drug can significantly reduce pain after hemorrhoidectomy; However, other studies have not confirmed the effect of oral metronidazole in reducing pain. The use of oral form has limitations compared to the local form due to its general effects. Therefore, in this study, the benefits of using metronidazole topical form in pain control after hemorrhoidectomy were evaluated.
Instrument and Methods
Study design
This cross-sectional descriptive study was conducted in 2019 in patients undergoing hemorrhoidectomy at Imam Reza Hospital (Tabriz University of Medical Sciences). Ninty-four individuals were selected by convenience sampling.
Inclusion/Exclusion Criteria
Inclusion criteria were age over 18 years, candidate for hemorrhoidectomy, grade 2, 3 and 4 hemorrhoids, clinically, having a fissure in the anal area. Exclusion criteria were cardiovascular disease, surgical site infection, anal abscess, and drug addiction.
Method of preparation of metronidazole ointment
First, metronidazole powder was prepared. Then, to prepare the ointment, several bases were used to knead the powder, including propylene glycol, liquid paraffin, glycerin and isopropyl alcohol, and among them, liquid paraffin was selected as the best material. Then metronidazole ointment was prepared with liquid paraffin based on Vaseline. In physico-chemical control experiments of the drug, to measure the amount of drug in the ointment, the spectroscopic method was performed at 319nm and the chemical stability of the ointment prepared by the accelerated method at four degrees (40, 50, 60 and 70) degrees. Celsius was performed and the half-life of the ointment at 25°C was determined to be 467 days. The microbial control of the product was performed according to the USP standard method and the microorganism did not grow in the culture medium.
Procedure
The prepared ointment was used by the surgeon after the surgery and before the dressing pack, then it was attached to the patient's file or cape and entered the ward with the patient and was given to the patient for later use. The patient was advised to rub 2 times a day for 2 weeks, each time the size of a fingertip equivalent to 2cm around the anus (not inside it). All patients within 24 hours after surgery with a prescription, including: laxative (MOM), the topical form of metronidazole or placebo were discharged. Most patients were advised to take acetaminophen codeine or a nonsteroidal anti-inflammatory drug if additional analgesia was needed. Patients' condition was assessed at intervals of 6 and 12 hours, as well as the first, second, seventh and fourteenth days after surgery. In this way, in the first hours after surgery (12, 6 and 24 hours) by evaluating the hospital and for later periods by visiting the office or by phone, the evaluation was done. VAS criterion was used to communicate with the patient and understand the severity and extent of pain according to the patient's ability to cooperate. Analgesic consumption was recorded in the first, second, seventh and fourth days after surgery. In this section, the patient was asked whether he uses oral painkillers or not, and if so, whether it has decreased or not.
Data analysis
The data were recorded in one form for each person and finally entered into SPSS 20 software; Frequency and percentage, mean and standard deviation were used to display the data. T-test was used to compare the severity of pain between the two groups at different times. P values less than 0.05 were considered significant.
Ethical considerations
Conscious consent was obtained from all patients. No cost was incurred from patients to participate in this study and to prepare metronidazole ointment. Patient information remained strictly confidential.
Findings
A total of 94 patients were included in the study, of which 70 were female and 24 were male. The female to male ratio was 20 to 5 in the metronidazole group and 30 to 14 in the placebo group. Fifty people in the metronidazel group with a mean age of 37 years (18 to 65 years) and 22 people in the placebo group with a mean age of 36 years (19 to 61 years) were evaluated. There was no significant difference between the two groups in terms of mean age (p=0.55).
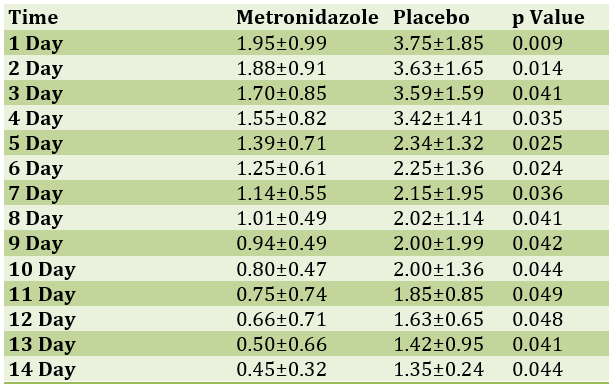
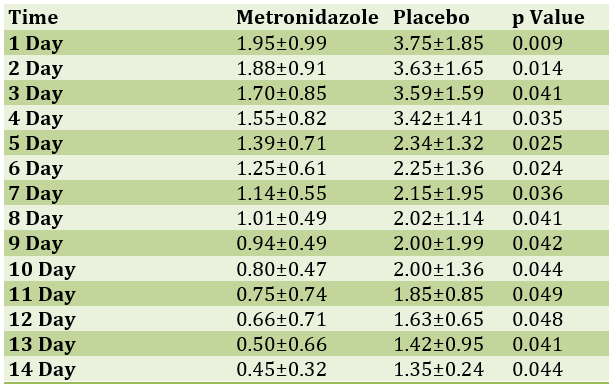
Topical form of metronidazole significantly reduced pain after hemorrhoidectomy compared with the placebo group in the sixth and twelfth hours (p=0.031 and p=0.001) and the first to fourteenth days after surgery, respectively (Tables 1 & 2).
Table 1) Comparison of postoperative pain in the two groups participating in the study (T-test)
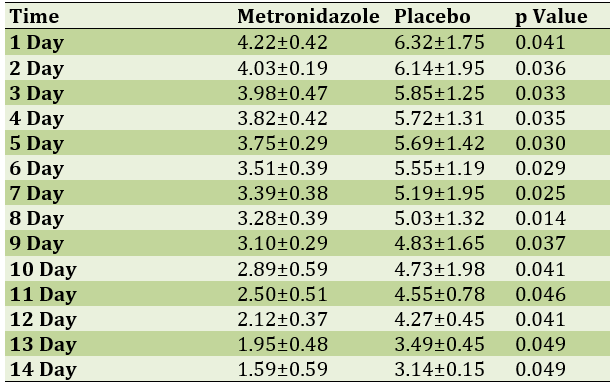
Table 2) Comparison of the amount of pain relieving drug between the two groups participating in the study (T-test)
Discussion
With home remedies and behavioral changes failing and correcting bad lifestyle habits, it is necessary to adopt medical methods to treat hemorrhoids. Of course, the choice of treatment also depends on the type and rate of disease progression, in the early stages of the disease, step-by-step treatment is usually chosen [11].
The main purpose of hemorrhoid medication is to control the acute symptoms of hemorrhoids instead of treating the disease itself [12]. In fact, hemorrhoids can only control the symptoms of the disease. Medications recommended for hemorrhoids are usually in the form of topical tablets, suppositories, and ointments [13].
Hemorrhoids occur as varicose veins in and around the anal vein, and a drug called Phlebotonics, which is made from plant extracts (containing flavonoids) and synthetic compounds, can help improve venous contractility, increase vasodilation, and increase permeability through an unspecified mechanism. Slowly It is also very effective in treating chronic venous insufficiency [14]. Statistics obtained in 2012 have proven the significant beneficial effects of this drug in controlling bleeding, itching and viscous discharge of this disease. It is also useful in reducing the symptoms after hemorrhoid surgery. Hydrocortisone and lidocaine are also temporary anti-inflammatory drugs that are effective in controlling pain and itching, but should not be taken permanently [15]. In this study, the topical form of metronidazole was able to significantly reduce postoperative pain in the metronidazole group compared with the placebo group. One of the possible reasons for the effect of metronidazole on the control of pain after hemorrhoidectomy is the direct anti-inflammatory effects of this drug, which can significantly reduce postoperative pain by reducing edema and premature inflammation of the surgical site [16]. Metronidazole reduces inflammation and postoperative pain by reducing the migration of neutrophils to the inflammatory site, inhibiting the production of hydrogen peroxide, hydroxyl radicals, and other oxidants that cause tissue damage in the area. These effects of the drug may justify pain control in the early hours of patients. Another reason for this finding may be related to the effects of this drug on anaerobic infections secondary to bacterial colonization in that area. The dimension also justifies the action [17]. A similar finding has been confirmed in another study [18]. Another important factor in the study of the effects of the drug is the effect on postoperative pain, which is one of the major problems of patients after hemorrhoidectomy [19]. The results of this study indicate a significant difference between the two groups at 48 hours after surgery, a finding that was not mentioned in other studies. The cause of this effect of the drug can also be attributed to the anti-inflammatory effects of the drug and the reduction of edema in the area of the antibiotic effect and the specific type of drug formulation (ointment) [20].
The small sample size of the participants in the study, as well as the failure to record the amount of activity after surgery, as well as the failure to record the duration of anesthesia and surgery were the limitations of this study; Due to the effectiveness of metronidazole ointment in reducing pain after hemorrhoidectomy, it is recommended to use this ointment to manage pain after surgery in these patients. However, further studies are needed for the widespread use of this form of medicine in the clinic.
Conclusion
Topical metronidazole can reduce postoperative pain. In addition, the pain after defecation and the need for analgesia are significantly reduced.
Acknowledgements: None declared by the authors.
Ethical Permission: This study was approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.1061).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
Hemorrhoid is one of the most common diseases of the gastrointestinal tract, which causes pain and bleeding due to local damage to the black veins in the anal area during defecation [1].
If this disorder is not controlled and treated on an outpatient basis, surgery is one of the good methods in treating hemorrhoids. But hemorrhoidectomy can also cause complications such as pain, bleeding, urinary retention, infection, compression and thickening of the stool, and damage to the internal sphincter [2]. In the meantime, it seems that several factors are involved in the occurrence of pain after hemorrhoidectomy, such as patient tolerance, type B anesthesia, postoperative analgesia, as well as surgical techniques [3, 4].
Therefore, in order for the patient to be able to tolerate this type of treatment, reducing the pain after hemorrhoids has always been an important goal [5]. Numerous studies have been performed to reduce pain after hemorrhoid surgery, including the use of 0.2% nitroglycerin ointment, which is helpful in relaxing the anal sphincter in the initial pain after hemorrhoidectomy, but the complication of headache following the use of this product appears sometimes unbearable for the patient and limits the use of this product [6].
Inhibition of the posterior areas around the anus by rupivacaine 0.75% to control pain, although it leads to an immediate analgesic effect, pain relief after surgery does not last long and is sometimes associated with serious problems [7, 8].
The use of fentanyl percutaneously and a subcutaneous morphine injection pump, despite effective pain control, can be costly and addictive. The use of botulinum toxin after hematoid hemorrhoids, although significantly reduces pain, due to the high cost of treatment and its injection by skilled professionals, it is not possible to use it for the general public [9, 10].
Recently, the use of metronidazole in reducing pain after hemorrhoids has been considered and it has been shown that the oral form of this drug can significantly reduce pain after hemorrhoidectomy; However, other studies have not confirmed the effect of oral metronidazole in reducing pain. The use of oral form has limitations compared to the local form due to its general effects. Therefore, in this study, the benefits of using metronidazole topical form in pain control after hemorrhoidectomy were evaluated.
Instrument and Methods
Study design
This cross-sectional descriptive study was conducted in 2019 in patients undergoing hemorrhoidectomy at Imam Reza Hospital (Tabriz University of Medical Sciences). Ninty-four individuals were selected by convenience sampling.
Inclusion/Exclusion Criteria
Inclusion criteria were age over 18 years, candidate for hemorrhoidectomy, grade 2, 3 and 4 hemorrhoids, clinically, having a fissure in the anal area. Exclusion criteria were cardiovascular disease, surgical site infection, anal abscess, and drug addiction.
Method of preparation of metronidazole ointment
First, metronidazole powder was prepared. Then, to prepare the ointment, several bases were used to knead the powder, including propylene glycol, liquid paraffin, glycerin and isopropyl alcohol, and among them, liquid paraffin was selected as the best material. Then metronidazole ointment was prepared with liquid paraffin based on Vaseline. In physico-chemical control experiments of the drug, to measure the amount of drug in the ointment, the spectroscopic method was performed at 319nm and the chemical stability of the ointment prepared by the accelerated method at four degrees (40, 50, 60 and 70) degrees. Celsius was performed and the half-life of the ointment at 25°C was determined to be 467 days. The microbial control of the product was performed according to the USP standard method and the microorganism did not grow in the culture medium.
Procedure
The prepared ointment was used by the surgeon after the surgery and before the dressing pack, then it was attached to the patient's file or cape and entered the ward with the patient and was given to the patient for later use. The patient was advised to rub 2 times a day for 2 weeks, each time the size of a fingertip equivalent to 2cm around the anus (not inside it). All patients within 24 hours after surgery with a prescription, including: laxative (MOM), the topical form of metronidazole or placebo were discharged. Most patients were advised to take acetaminophen codeine or a nonsteroidal anti-inflammatory drug if additional analgesia was needed. Patients' condition was assessed at intervals of 6 and 12 hours, as well as the first, second, seventh and fourteenth days after surgery. In this way, in the first hours after surgery (12, 6 and 24 hours) by evaluating the hospital and for later periods by visiting the office or by phone, the evaluation was done. VAS criterion was used to communicate with the patient and understand the severity and extent of pain according to the patient's ability to cooperate. Analgesic consumption was recorded in the first, second, seventh and fourth days after surgery. In this section, the patient was asked whether he uses oral painkillers or not, and if so, whether it has decreased or not.
Data analysis
The data were recorded in one form for each person and finally entered into SPSS 20 software; Frequency and percentage, mean and standard deviation were used to display the data. T-test was used to compare the severity of pain between the two groups at different times. P values less than 0.05 were considered significant.
Ethical considerations
Conscious consent was obtained from all patients. No cost was incurred from patients to participate in this study and to prepare metronidazole ointment. Patient information remained strictly confidential.
Findings
A total of 94 patients were included in the study, of which 70 were female and 24 were male. The female to male ratio was 20 to 5 in the metronidazole group and 30 to 14 in the placebo group. Fifty people in the metronidazel group with a mean age of 37 years (18 to 65 years) and 22 people in the placebo group with a mean age of 36 years (19 to 61 years) were evaluated. There was no significant difference between the two groups in terms of mean age (p=0.55).
Topical form of metronidazole significantly reduced pain after hemorrhoidectomy compared with the placebo group in the sixth and twelfth hours (p=0.031 and p=0.001) and the first to fourteenth days after surgery, respectively (Tables 1 & 2).
Table 1) Comparison of postoperative pain in the two groups participating in the study (T-test)
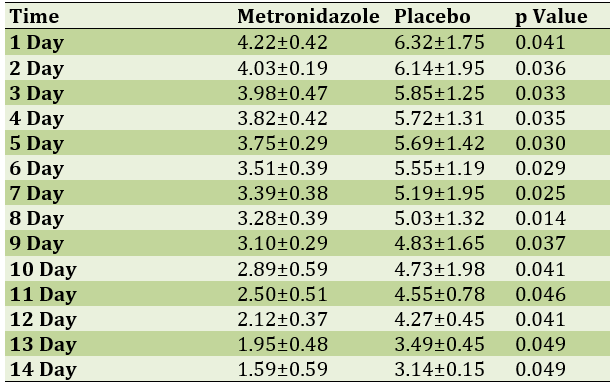
Table 2) Comparison of the amount of pain relieving drug between the two groups participating in the study (T-test)
Discussion
With home remedies and behavioral changes failing and correcting bad lifestyle habits, it is necessary to adopt medical methods to treat hemorrhoids. Of course, the choice of treatment also depends on the type and rate of disease progression, in the early stages of the disease, step-by-step treatment is usually chosen [11].
The main purpose of hemorrhoid medication is to control the acute symptoms of hemorrhoids instead of treating the disease itself [12]. In fact, hemorrhoids can only control the symptoms of the disease. Medications recommended for hemorrhoids are usually in the form of topical tablets, suppositories, and ointments [13].
Hemorrhoids occur as varicose veins in and around the anal vein, and a drug called Phlebotonics, which is made from plant extracts (containing flavonoids) and synthetic compounds, can help improve venous contractility, increase vasodilation, and increase permeability through an unspecified mechanism. Slowly It is also very effective in treating chronic venous insufficiency [14]. Statistics obtained in 2012 have proven the significant beneficial effects of this drug in controlling bleeding, itching and viscous discharge of this disease. It is also useful in reducing the symptoms after hemorrhoid surgery. Hydrocortisone and lidocaine are also temporary anti-inflammatory drugs that are effective in controlling pain and itching, but should not be taken permanently [15]. In this study, the topical form of metronidazole was able to significantly reduce postoperative pain in the metronidazole group compared with the placebo group. One of the possible reasons for the effect of metronidazole on the control of pain after hemorrhoidectomy is the direct anti-inflammatory effects of this drug, which can significantly reduce postoperative pain by reducing edema and premature inflammation of the surgical site [16]. Metronidazole reduces inflammation and postoperative pain by reducing the migration of neutrophils to the inflammatory site, inhibiting the production of hydrogen peroxide, hydroxyl radicals, and other oxidants that cause tissue damage in the area. These effects of the drug may justify pain control in the early hours of patients. Another reason for this finding may be related to the effects of this drug on anaerobic infections secondary to bacterial colonization in that area. The dimension also justifies the action [17]. A similar finding has been confirmed in another study [18]. Another important factor in the study of the effects of the drug is the effect on postoperative pain, which is one of the major problems of patients after hemorrhoidectomy [19]. The results of this study indicate a significant difference between the two groups at 48 hours after surgery, a finding that was not mentioned in other studies. The cause of this effect of the drug can also be attributed to the anti-inflammatory effects of the drug and the reduction of edema in the area of the antibiotic effect and the specific type of drug formulation (ointment) [20].
The small sample size of the participants in the study, as well as the failure to record the amount of activity after surgery, as well as the failure to record the duration of anesthesia and surgery were the limitations of this study; Due to the effectiveness of metronidazole ointment in reducing pain after hemorrhoidectomy, it is recommended to use this ointment to manage pain after surgery in these patients. However, further studies are needed for the widespread use of this form of medicine in the clinic.
Conclusion
Topical metronidazole can reduce postoperative pain. In addition, the pain after defecation and the need for analgesia are significantly reduced.
Acknowledgements: None declared by the authors.
Ethical Permission: This study was approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.1061).
Conflicts of Interests: None declared by the authors.
Funding/Support: None declared by the authors.
References
1. Neogi P, Sinha A, Singh M. Is metronidazole a panacea for post-hemorrhoidectomy pain?. Int Surg J. 2018;5(11):3598-601. [Link] [DOI:10.18203/2349-2902.isj20184629]
2. Wanis KN, Emmerton-Coughlin HM, Coughlin S, Foley N, Vinden C. Systemic Metronidazole May Not Reduce Posthemorrhoidectomy Pain: A Meta-Analysis of Randomized Controlled Trials. Dis Colon Rectum. 2017;60(4):446-55. [Link] [DOI:10.1097/DCR.0000000000000792]
3. Ypsilantis E, Carapeti E, Chan S. The use of topical 10% metronidazole in the treatment of non-healing pilonidal sinus wounds after surgery. Int J Colorectal. Dis. 2016;31(3):765-7. [Link] [DOI:10.1007/s00384-015-2269-8]
4. Watson AJ, Hudson J, Wood J, Kilonzo M, Brown SR, McDonald A, et al. Comparison of stapled haemorrhoidopexy with traditional excisional surgery for haemorrhoidal disease (eTHoS): A pragmatic, multicentre, randomised controlled trial. Lancet. 2016;388(10058):2375-85. [Link] [DOI:10.1016/S0140-6736(16)31803-7]
5. Davis BR, Lee -Kong SA, Migaly J, Feingold DL, Steele SR. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids. Dis Colon Rectum. 2018;61(3):284-92. [Link] [DOI:10.1097/DCR.0000000000001030]
6. Rudd RA, Aleshire N, Zibbell JE, Matthew Gladden R. Increases in drug and opioid overdose deaths-United States, 2000-2014. Am J Transplant. 2016;16:1323-7. [Link] [DOI:10.1111/ajt.13776]
7. Sammour T, Barazanchi AW, Hill AG, Prospect Group (Collaborators). Evidence-based management of pain after excisional haemorrhoidectomy surgery: A prospect review update. World J Surg. 2017;41(2):603-14. [Link] [DOI:10.1007/s00268-016-3737-1]
8. Huang YJ, Chen CY, Chen RJ, Kang YN, Wei PL. Topical diltiazem ointment in post-hemorrhoidectomy pain relief: A meta-analysis of randomized controlled trial. Asian J Surg, 2018;41(5):431-7. [Link] [DOI:10.1016/j.asjsur.2017.06.002]
9. Liu JW, Lin CC, Kiu KT, Wang CY, Tam KW. Effect of Glyceryl Trinitrate Ointment on Pain Control After Hemorrhoidectomy: A Meta-analysis of Randomized Controlled Trials. World J Surg. 2016;40(1):215-24. [Link] [DOI:10.1007/s00268-015-3344-6]
10. Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [Link] [DOI:10.1136/bmj.l4898]
11. Rodriguez-Wong U, Ocharan-Hernandez ME, Toscano-Garibay J. Topical diltiazem for pain after closed hemorrhoidectomy. Rev Gastroenterol Mex. 2016;81(2):74-9. [Link] [DOI:10.1016/j.rgmxen.2016.03.003]
12. Rodriguez-Wong U, Rodriguez-Medina U, Medina-Murillo GR. Randomized clinical trial with topical diltiazem for post-hemorrhoidectomy wound healing. Rev Gastroenterol Mex. 2019;84(1):119-22. [Link] [DOI:10.1016/j.rgmxen.2019.01.003]
13. Yadav S, Khandelwal RG, Om P, Ravindra K, Choudhary KL. A prospective randomized double-blind study of pain control by topical calcium channel blockers versus placebo after Milligan-Morgan hemorrhoidectomy. Int J Color Dis. 2018;33(7):895-9. [Link] [DOI:10.1007/s00384-018-3067-x]
14. Ala S, Alvandipour M, Saeedi M, Hamidian M, Shiva A, Rahmani N, et al. Effects of Topical Atorvastatin (2 %) on Posthemorrhoidectomy Pain and Wound Healing: A Randomized Double-Blind Placebo-Controlled Clinical Trial. World J Surg. 2017;41(2):596-602. [Link] [DOI:10.1007/s00268-016-3749-x]
15. Ala S, Alvandipour M, Saeedi M, Mansourifar M, Monajati M, Shiva A. Effect of Topical Baclofen 5% on Post-Hemorrhoidectomy Pain: Randomized Double Blind Placebo-Controlled Clinical Trial. J Gastrointest Surg. 2019;24(2):405-10. [Link] [DOI:10.1007/s11605-019-04147-7]
16. Xia W, Manning JP, Barazanchi AW, Su'a B, Hill AG. Metronidazole following excisional haemorrhoidectomy: a systematic review and meta-analysis. ANZ J Surg. 2018;88(5):408-14. [Link] [DOI:10.1111/ans.14236]
17. Davis BR, Lee-Kong SA, Migaly J, Feingold DL, Steele SR. The American society of colon and rectal surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum. 2018;61(3): 284-92. [Link] [DOI:10.1097/DCR.0000000000001030]
18. Neogi P, Sinha A, Singh M. Is metronidazole a panacea for post-hemorrhoidectomy pain?. Int Surg J. 2018;5(11):3598-601. [Link] [DOI:10.18203/2349-2902.isj20184629]
19. Ebied EF, Darweesh AA, Khalil AA, Nma SM. Assessment of oral metronidazole in pain management post Haemorrhoidectomy. Egypt. J. Hosp. Med. 2018; 73(1):5940-33. [Link] [DOI:10.21608/ejhm.2018.12064]
20. Xia W, Manning JP, Barazanchi AW, Su'a B, Hill AG. Metronidazole following excisional haemorrhoidectomy: A systematic review and meta-analysis. ANZ J Surg. 2018;88(5):408-14. [Link] [DOI:10.1111/ans.14236]









